
Dracunculus medinensis
- Dracunuculus medinensis is among the longest nematodes affecting humans.
- It is also known as Guinea worm, Medina worm, serpent worm or dragon worm.
- It causes dracunculiasis or dracontiasis, a nodular dermatosis produced by the development of Dracunculus parasite in the subcutaneous tissue.
Habitat:
- The adult females inhabit the subcutaneous tissue usually of the foot or lower limbs.
- Less frequently they also inhabit other parts of the body including the head and neck.
Morphology:
Adult worms
- Male:
- Male worms are difficult to demonstrate as they are immediately after fertilizing the females. Hence, it has not yet been recovered from man.
- The male measures 12-30 mm in length and 0.4 mm in breadth.
- Female:
- It is slender long worm and is one of the longest nematodes known to cause infection in man.
- It measures 60 cm to 1 mm or more in length and 1.5 to 1.7 mm in diameter, resembling a piece of long twine thread.
- The body is cylindrical, smooth and milk white in color.
- The posterior end is extremely tapering and is bent to form a hook.
- A minute triangular mouth is present in an anterior end.
- An inner layer of 4 papillae-6 papillae and outer layer of 4 pairs of papillae surrounded the mouth.
- A pair of uteri, oviducts and tubules and a single unpaired vagina constitutes the female genital tract.
- The worm is ovoviviparous and discharge embryos in successive batches for a period of about 3 weeks until the gravid female completely implies its uterine contents.
- The body fluid is toxic and causes a bluster if female escapes into the tissue.The life span of female is about 1 year and that of the male is not more than 6 months.
larva:
- First stage Larva
- It is unsheathed and coiled with a round anterior end and a long slender filariform tail.
- It is large, measuring 650-750 mm in length and 17-20 mm in breadth.
- The cuticle is conspicuously striated.
- It moves about with a shift motion, briskly coiling and uncoiling body.
- It shows a tad-pole like movement in water.
- These larva are set free only at the time of partition when the affected part is submerged in water.
- Further development proceeds in the body of a minute fresh water crustacean of the genus Cylops.
- Third stage of larva:
- It is the infective stage of the parasite.
- It is found in the body cavity of Cyclops.
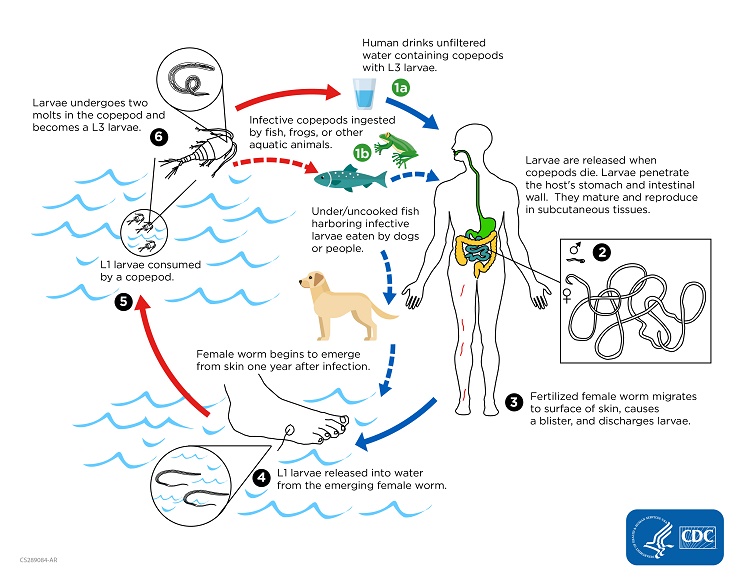
Life cycle of Dracunuculus medinensis :
- Lifecycle is completed in two hosts:
- Definitive host: Human
- Intermediate host: Cyclops and other twelve species.
- Entrance into man and development into adult worms:
- Man acquires infections by drinking unfiltered water containing infected Cyclops.
- On reaching the stomach, the cyclopses are digested by the gastric juices and L3 larva are liberated.
- The larva penetrated the gut wall and enter the retroperitoneal connective tissue where they grow and becomes sexually mature.
- The males die after fertilizing the females and disappear within 6 months of infection.
- The gravid female migrates and selects those parts of the skin labile to come in contact with water such as the backs of water carriers, anus and legs of washer men and legs of those who fill water in containers in ‘step wells’ and ponds.
- On reaching the skin surface, it secretes a toxin, producing a blister which later ruptures and forms an ulcer, contact with water stimulates the worm to protrude its head through the center of the ulcer and causes a reflex discharge of a milky fluid containing large number of first stage rhabditiform larva.
- Development of larva in Cyclops:
- The larva discharged in water swims vigorously in water with tad-pole like movement.
- These larvae further develop when ingested by suitable Cyclops species.
- In the body cavity of Cyclops, the first stage larva moults twice to develop into third stage larva, the infection from the parasite.
- These infected Cyclops have short life span than normal non infected ones.
- The infected Cyclops harboring third stage larva are infective to man and the cycle is repeated.
Mode of transmission:
- Water containing infected Cyclops is the main source of infection.
- Man acquires infections by drinking water contaminated with Cyclops harboring third stage larva.
Pathogenesis:
- The third stage larva are not pathogenesis and do not produce any pathological lesions.
- Only female adult worm is pathogenic.
- It produces a toxin, forming blister which is formed at the site at which the female worm comes out of the surface of the skin on coming contact with water.
- The blister is filled with the fluid which is bacteriologically sterile and contains numerous larvae and leucocytes.
- Diffusible toxins produced by the parasite are believed to cause urticaria, dyspnea, vomiting, mild fever and occasional fainting.
Clinical manifestation:
- The pre-patent period is 10-14 months.
- The symptoms are manifested during parturition of the female and are due to the liberation of a toxic substance causing allergic manifestation and blister formation.
- Septic infection can occur as a result of contamination by secondary organisms drawn in by the worm at the time of retraction.
- Blister formation appears wherever the female worms make an attempt to come to the surface of the body where it can readily discharge its larva.
- The blister is usually found on the lower extremities of the body especially between the metatarsal bones, sole of the feet or on the ankle and less frequently in arms, buttock, scrotum, head, neck and female breast.
- Blister formation is accompanied by intense burning pain, ‘fiery serpent’.
- This may be accompanied by generalized reactions such as urticaria, nausea, vomiting, diarrhea and giddiness and marked burning sensation over the next few days the lesions vesiculates and blister ruptures producing a painful ulcer.
- The worm is often visible in the opening of ulcer.
- If the female worms break during the attempts of extractions the larva remain trapped in the subcutaneous tissue and may give rise to cellulitis and abscesses.
- In uncomplicated cases, lesions may only last for several weeks until the worm is completely expelled.
- However, many cases infection of the worm track with persistence of the lesions, chronic ulceration and possible sequelae, involving disseminated infection, phlegma of limbs, contractures of tendons, fibrous ankylosis or arthritis in the joints, die prematurely and calcify. The calcified worms can be trigger arthritis, locked joints or permanent clipping and deformations.
Laboratory diagnosis:
- Detection of adult worms:
- This is possible when the female worm appears at the surface of the skin.
- Detection of first stage larva:
- Specific diagnosis is made by the microscopic demonstration of the first stage larva in the discharge fluid.
- Intradermal test:
- Infection of Dracunculus antigens intradermally causes a wheal to appear in the course of 24 hours in positive cases.
- X-ray examination:
- Worms in deeper tissue after the death either become calcified or absorbed.
- The position of calcified worm may be located by skiagraphy.
- Blood examination
- Serodiagnosis:
- IFA, IHA, ELISA and western blot are the frequently used test for demonstration of circulating antibodies in the serum for diagnosis of dracunculiasis.
Treatment:
- There is no specific drugs or medicines to treat or prevent the disease.
- The mainstay of treatment is the extractions of the adult worm from the patient using a stick at the surface and wrapping the worm or few cm per day.
- Full extraction can take several days or weeks.
- Topical antibodies are applied to prevent secondary bacterial infections and the affected body part is bandaged with fresh gauze to protect the site.
- Surgical removal of worm using local anesthesia is another method of treatment
- Albendazole, Mebendazole, Niridazole, thiabendazole and metronidazole are used as anti-inflammatory agents.
- Analgesics such as aspirin or ibuprofen are given to help reduce the pain and inflammation.
Prevention and control:
- The disease can be transmitted only by drinking contaminated water and can be completely prevented through to relatively simple measures.
- Preventing people from drinking Cyclops contaminated water:
- Avoid drinking contaminated water
- Filtering water
- Boiling
- Treatment of water with larvicides to kill Cyclops
- Preventing people infected with the worm from entering water sources used for drinking.
Epidemiology
- D. medinensis infection is reported from 18 century of the world.
- The infection is particularly wide spread in Africa and middle east.
- About 140 million people are estimated to suffer from dracunculiasis.
