Hookworms:
- Hookworms are parasitic nematode that lives in the small intestine of mammalian host such as dog, cat or humans.
- They are characterized by their presence of well-defined buccal capsules bearing clotting plates and teeth.
- Two species of hookworms, commonly infect humans:
- Ancylostoma duodenale
- Necator americanus
- Ancylostoma duodenale, also known as the old hookworm is a common hookworm of human.
- It causes ancylostomiasis in humans, characterized by non-deficiency anemia and hypoalbuminemia.
- Necator americanus also known as the New World hookworm is another cause of hookworm disease in humans.
- Necatoriasis is the term for the condition of being host to an infestation of a species of Necator.
Habitat:
- The adult worm lives in the small intestine of a man particularly in the jejunum, less often in the duodenum and rarely in the ileum.
Morphology: Ancyclostoma duodenale
Adult worm:
- It is small greyish white, cylindrical worm.
- When freshly passed the worm has a reddish-brown color due to the ingested blood in intestinal tract.
- The anterior end of the worm is bent slightly in the same direction of the body curve resembling a hook, hence they are called hookworms.
- The large and conspicuous buccal capsule is lined with a hard substance
- The buccal capsule is provided with 6 teeth, 4-hook like on the ventral surface and had a pair of knob-like (triangular plates) on the dorsal surface.
- There are five glands connected with the digestive system:
- one of them called the esophageal gland, secretes a ferment which prevents the clotting of blood.
- The sexes are easily differentiated by their size, the shape of the tail and position of the genital opening.
- Male:
- shorter, measuring 8mm in length, the posterior end is expanded in an umbrella like fashion (copulatory bursa).
- -Genital opening is present posteriorly and opens with the cloaca.
- Female:
- longer than males, measuring 12.5 mm in length.
- The posterior end is tapering and possess no bursa.
- The genital pore is present at the junction of posterior and middle third of the body.
- Owing to the position of the genital opening, the worm assumes the Y-shaped figure during copulation.
- Copulatory bursa in males is characteristic bell shaped used to catch and hold the female nematode during mating.
- – It is membranous, asymmetrical and consists of 13 fingers like rays in 3 lobes: 1 dorsal and 2 lateral.
- -Dorsal lobe consists 3 (1 single dorsal ray and 2 external dorsal rays: the two lateral lobes contain 1/3 pairs of lateral rays and 2 pairs of ventral rays).
Eggs:
- Eggs are oval in shape.
- 60 mm in length and 40 mm in breadth colorless.
- They are surrounded by a transparent hyaline shell-membrane.
- Eggs contain an un-segmented ovum usually with 4 blastomeres.
- A clear space is present between the egg shell and segmented ovum.
- These eggs floats in saturated solution of common salt.
- The eggs of Necator is slightly smaller than Ancylostoma.
- The female Ancylostoma produces 10,000-20,000 eggs per day whereas N. americanus produce less eggs i.e. 3000-6000 per day.
Filariform larva:
- It is the non-feeding form of the worm and is the infective form of the parasite.
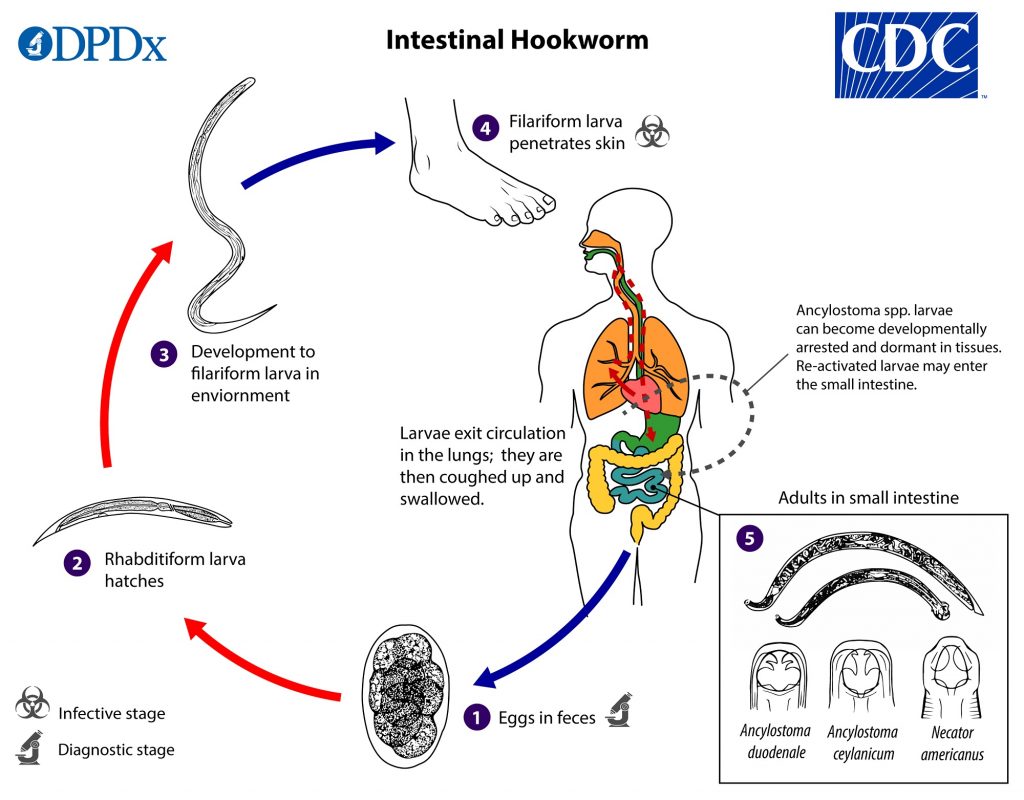
Life cycle:
- The life cycle of the two species of hook worm are same.
- The only difference is the morphology of filariform larva.
- Life cycle is completed in a single host, the man. No other intermediate host is required.
- The following are the various stages of the life cycle:
- Stage 1: Passage of eggs from the infected host
- The eggs containing segmented oval with 4 blastomeres, are passed out in the feces of human host.
- Stage 2: Development in soil
- Eggs under the favorable conditions (damp, warm, well-oxygenated soil) hatch to rhabditiform larva (250mm in length) i.e. L1 larva within 48 hours.
- The rhabditiform larva moults twice, on the 3rd and 5th day to develop into a filariform larva (500—600 mm in length), the infective stage of the parasite.
- The time taken for development from eggs to filariform larva is on an average 8-10 days.
- Stage 3: Entrance to new host
- The L3 larva cast of their sheath and gain entrance into the body by penetrating the skin, through the epidermis to dermis and subcutaneous tissue.
- Stage4: Migration
- On reaching the subcutaneous tissue, the larva enters into the lymphatic small vessels.
- They pass through the lymph-vascular system into the venom circulation and carried via the right heart into the pulmonary capillaries.
- They break the lung capillaries and enter into the alveolar spaces.
- They then ascend upward the bronchial tree to trachea and larynx, crawl up over the epiglottis to the back of pharynx and ultimately swallowed.
- During migration or entering the esophagus, the larva undergoes a third moult to form fourth stage (L4 larva) equipped with a buccal capsule allowing adherence to the gut wall.
- Stage5: Localization and laying of eggs
- The growing larva settle down in the small intestine, undergo a fourth moult to develop into an adolescent worm.
- At this stage, the provisional toothless buccal capsule formed is cast off and definitive buccal capsule complete with teeth is formed.
- During 4-5 weeks, the adults who remain attached to mucosa of the small intestine becomes sexually mature.
- The fertilized females begin to lay eggs which are excreted out in the feces.
- The cycle is thus repeated.
- The interval between the time of skin infection and the first appearance of eggs in feces is about 6 weeks.
Mode of transmission:
- Human feces are the only source of infection.
- The route of infection transmission:
- Cutaneous route: Penetration of the skin by infective filariform larva
- Oral route: Ingestion of L3 larva present in the soil, occurs less frequency. Larva in mouth develops directly into adult worms.
- Transmammary transmission: Breast feeding by mothers to infants.
- Very rarely, trans-parental transmission.
Pathogenesis:
Pathogenicity of adult worm:
- The major pathological changes in ancyclostomiasis are caused by the attachment of adult worms to the intestinal walls by their buccal capsule.
- The common site of infection is the upper small intestine.
- The attachment of parasite leads to mechanical disruption of intestinal mucosa of the resulting ‘mucosal plug’ lodged within the worm’s buccal capsule.
- These parasites penetrate the blood vessels with their mouth parts and suck the blood to get the nutrition.
- These worms cause considerable loss of blood and tissue.
- The adult Ancylostoma can suck about 0.2 ml blood a day while smaller Necator suck about 0.03 ml per day.
- The secretions of the site may continue for sometimes, this add to blood loss.
- Excessive blood loss caused by heavy and prolonged worm infection leads to hypochromic microcytic anemia.
Pathogenicity of infective larva:
- The infective filariform larva at the site of the penetration of the skin, produce a local reaction called ground itch.
- This allergic manifestation is more severe in Necator infection
- In previously sensitized host, it can lead to secondary bacterial infections.
- The migration of large no. of larva, through the lung produces minute hemorrhage and infiltration of leucocytes resulting in the entrapment of the larva in lung tissue.
- Both eosinophilia and leukocytosis occur at this stage.
Clinical manifestation:
The clinical symptoms depend on the site where the worms are present and their burden.
1. Skin infection:
- Hookworm related cutaneous larva migrans (HrCLM) is a parasitic skin disease caused by migration of hookworm larva in the epidermis.
- Ground itch is the early clinical manifestation during the penetration of L3 larva on the skin. It is believed to be due to allergic components of the larva.
- Lesions are characteristically seen in and around feet particularly between the toes.
- It is associated with intense itching, edema and erythema and rash.
- The associated secondary bacterial infection is more common during this stage.
2. Pulmonary infection:
- It is associated with low grade fever, mild cough dizziness and hemolysis.
- Pneumonia with pulmonary consolidation is seen in persons with severe infection.
3. Intestinal infection:
- Acute intestinal symptoms such as abdominal pain, nausea, vomiting and hemorrhagic diarrhea are observed.
- Chronic hook worm disease is characterized by blood loss and Ion-deficiency anemia and is associated with fatigue, pallor, tachycardia and dyspnea on exertion.
- Hypoproteinemia may cause edema and there can be sign of malabsorption and malnutrition.
- In children there may also be adverse effects on physical growth and intellectual growth.
- The severity of the disease varies with the worm burden and the amount of blood lost heavy infections can be fatal, particularly in infants.
Laboratory diagnosis:
- Specimen:
- Stool, duodenal content obtained by the duodenal intubation (Ryles tube) may sometimes reveal either egg or the adult worms.
1. Stool microscopy:
- A specific diagnosis of hookworm infection is based on the microscopic identification of eggs.
- This is carried out by examination of a direct wet mount of the stool.
- In case of light hook worm infection, detection of eggs can be done using concentration methods-formalin ether concentration technique or simple salt floatation technique.
- Kato-Katz is a useful method for quantitation estimation of hook worm eggs present in the stool.
- The intensity of the infection is determined by counting the no. of eggs in a measured volume of feces.
2. Stool culture:
- Harada- mori method of culture of stool is carried out to demonstrate L3 larva.
- The eggs present in the stool are smeared in moist filter paper, after an incubation of 5-7 days at room temperature, L3 larva hatch out of eggs.
3. Imaging methods:
- On chest X-ray a patchy infiltrate may be demonstrated in the migratory phase of larva in the lungs.
4. Blood test:
- This is carried out to ascertain the nature of anemia and the presence of eosinophilia.
5. Occult blood test:
- occult blood in the stool gives a position reaction in case of hookworm infection
- Charcot-Leyden crystals are often found in the stool.
Treatment:
- Mebendazole is a drug of choice- oral, 100 mg twice daily for 3 days
- Others anti parasitic drugs are- pyrantel pamoate, thiabendazole, Albendazole, levamisole
- Treatment of iron deficiency anemia with replacement iron therapy.
Prevention:
- Sanitary disposal of human feces
- Treatment of infected persons.
- Use of sanitary latrines, use of foot wears.
- Health education with improved nutrition supplemented with the dietary iron.
Epidemiology:
- Hookworm infections are the second most common helminthic infection next to ascariasis.
- The infection in worldwide is distribution more commonly in areas with warm and moist climate.
- Approx. 1200 million people are infected worldwide.
- Ancylostoma is found in Europe around the Mediterranean, on the west of South America and in parts of China, India and Nepal.
- Necator is found much over of the western Hemisphere, Africa and South East Asia.
