Type I hypersensitivity reaction: mechanism and clinical manifestation
- Type-I hypersensitivity reaction is an immediate type of reaction mediated by IgE.
- It is also known as anaphylactic reaction or allergy. It is induced by certain types of antigen called allergens such as pollengrains, dandruff, dusts, food components etc.
- Allergens induces humoral antibody response by the same mechanism as other soluble antigens in the generation of antibody secreting plasma cells and memory cells but the difference is that the plasma cell secretes IgE class of antibody.
- This IgE class of antibodies have high binding affinity to Fc receptor on the surface of tissue mast cells and blood basophils. Mast cells and basophils bound by IgE are said to be sensitized.
- A latter exposure to the same allergens cross links the membrane bound IgE on sensitized mast cell and basophils causing degranulation of these cells.
- Degranulation causes release of pharmacological active mediators which act on surrounding tissue causing vasodilation and smooth muscle contraction which may be either systemic or localized. This effect is also termed as Allergy.
Mechanism of Type I hypersesnsitivity reaction:
Development of allergy or anaphylactic reaction requires two dose of antigen. 1st dose is known as sensitizing dose and 2nd dose is known as shocking dose.
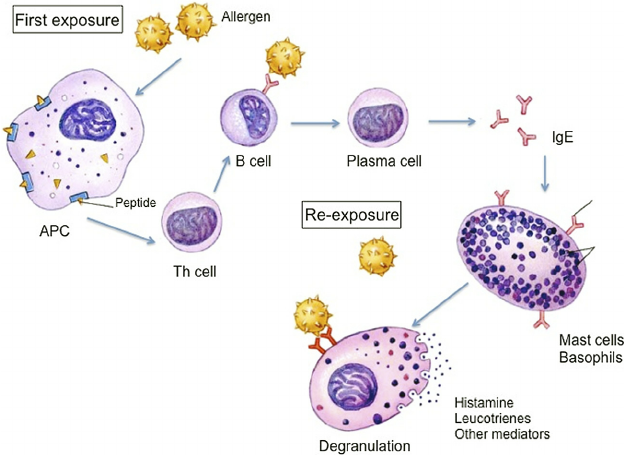
1. Production of IgE antibody:
- When antigen (allergen) enters into host production of antibody begins.
- At first allergen is processed and presented by antigen presenting cells (APCs) to CD4 T cells.
- Activated CD4 t cells divides to form T helper cell and memory cell. T helper produces IL4.
- At the same time B cell bind to antigen in presence of APC and IL4 and gets activated.
- Activated B cells divide to form plasma cells and memory cells.
- Up to this step, mechanism is similar to that of normal humoral immune response. The difference between Type I hypersensitivity and normal immune response is that the plasma cell produces IgE antibody instead of Ig M or IgG.
2. Sensitization:
- Fc region of IgE antibody has receptor on the surface of tissue mast cells and blood basophils. So the IgE antibody binds to FcRI of mast cells and basophils.
- This binding of IgE to mast cell and basophil is known as Sensitization and the mast cells and basophils are said to be sensitized.
3. Shocking dose of antigen:
- When the same antigen (allergen) enter into same host for second time in life, antigen cross linked with Fab region of IgE molecules on the surface of mast cell or basophils.
4. Degranulation of mast cell:
- The cross-linking of antigen (allergen) to IgE antibody causes degradation of mast cell and basophils releasing various pharmacological active chemicals such as histamine, heparin, serotonin, cytokines, leucotriene, prostaglandin etc.
5. Anaphylatic reaction:
- These active chemical mediators acts on surrounding tissue producing various symptoms of allergy such as vasodylation, smooth muscle contraction, mucus production, sneezing, etc.
- The allergic reaction may be localized or systemic depending upon types of allergen.
Mechanism of Activation and Degranulation of mast cell:
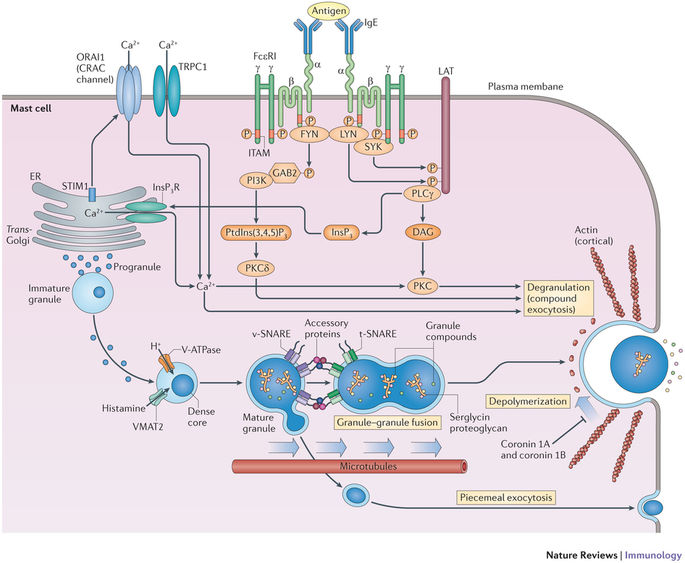
The intracellular signelling events that ultimately results in mast cell degranulation are manifested involving cooperation among various protein and lipid kinase and phosphatase and rearrangement of cytoskeleton.
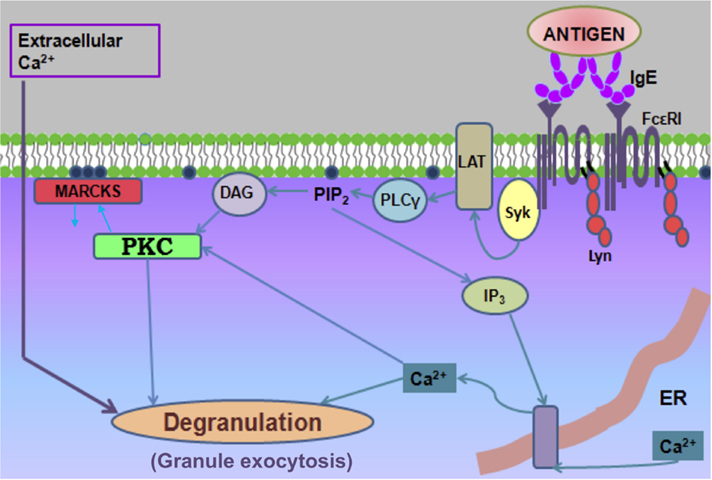
The biochemical events in mast cell activation and degranulation can be divided into 3 steps.
- Phosphorylation
- Methylation
- Adenylation
Phosphorylation:
- Binding of alleging on FcERI bounded antibody activates protein tyrosine kinase (PTK).
- PTK then phosphorylates phospholipase C which converts phosphatidylinositol 4,5 bisphosphate (PIP2) into diacetylglycerol (DAG) and inositol triphosphate (IP3).
- IP3 is a potent mobilize which causes pore formation and release Ca++ ions
- DAG activates protein kinase c (PKC).
Methylation:
- Cross linakage of FcERI also activates an enzyme that converts phosphatidyl serine (PS) into phosphatidylethanolamine (PE).
- Eventually PE is methylated to form phosphotidyl choline (PC) by the enzyme phopholipid methyl transferase I and II (PMT I and PMT II).
- The accumulation of PC on exterior surface of plasma membrane causes an increased membrane fluidity and facilitates the formation of Ca++ channel and Ca++ ions enter through the channel.
- Ca++ ion and PTK activates Mitoegn-activated protein kinase (MAPK).
- MAPK activates phopolipase A2 which promotes breakdown of phosphotidyl cholone (PC) into Lyso PC and Arachidonic acid.
- Arachidonic acid is converted into potent mediator Leckotrines and prostaglandin D2.
- Activated MAPK also induces secretion of cytokines by increasing transcription of cytokine genes.
Adenylation:
- FcERI cross linkage also activates the membrane adenylate cyclase enzyme leading to transient increase of cAMP within 15 seconds.
- A later drop in cAMP is mediated by protein kinase and is required for degranulation of mast cell.
- cAMP dependent protein kinase phosphorylates the granule membrane protein, thereby changing the permeability of the granules to water and Ca++ ions causing swelling of granules.
- Consequently swelling of granules and formation of Soluble N-ethylmaleimid attachment receptor (SNARE) protein complex, facilitates fusion of membrane and release of pharmacological chemical products, which is responsible for allergic symptoms.
Clinical manifestation of Type I hypersensitivity reaction:
Clinical symptoms ranges from life threatening conditions such as systemic anaphylaxis and severe asthma to localized reaction such as hey fever and eczema.
i. Systemic anaphylaxis:
- It is a shock like and often fatal state, which is usually initiated by allergen directly into blood stream or absorbed from gut or skin.
The symptoms are;
- Labored breathing
- Drop in blood pressure
- Smooth muscle contraction
- Bronchiole constriction
- Suffocation
ii. Localized hypersensitivity:
- It is limited to specific target tissue or organs, often involving epithelial surface at the site of allergen entry.
- The tendency to manifests hypersensitivity reaction is inherited and is called atopy.
Atopic allergy includes wide range of IgE mediated disorders such as:
- Hey fever (allergic rhinitis)
- Asthma (allergic or intrinsic)
- Food allergy
- Atopic dermatitis (eczema)
