Influenza virus
- The family Orthomyxoviridae contains a single genus Influenza virus with three types-A, B and C. Influenza viruses are classic respiratory viruses. They cause influenza, an acute infections disease of the respiratory tract that occurs in sporadic, epidemic and pandemic forms
- A unique feature of influenza virus is its ability to undergo antigenic variations. The surface glycoprotein (Haemagglutinin and Neuraminidase) show variations and are primarily responsible for antigenic variations. Antigenic variability is highest in influenza virus type A and less in type B, while it has not been demonstrated in types C.
Structure of Influenza virus
- Shape:
- The influenza virus particle is typically spherical with a diameter of about 80-120 mm but pleomorphism is common.
- Filamentous forms upto several micrometers in length and readily visible under the dark ground microscope are frequent seen in freshly isolated strains.
- Symmetry:
- The virus is core consists of ribonucleoprotien in helical symmetry.
- The nucleoprotein (NP) associates with the viral RNA to form a ribonucleoprotein (RNP) which is a structure of 9 mm in diameter that assumes a helical configuration and forms the viral nucleocapsid.
- Genome and protein:
- Influenza virus contains negative sense single stranded RNA (-ssRNA) genome which is segmented.
- Type A and B influenza virus consist of 8 pieces of segmented RNA (while type C influenza virus contains 7 segments), which encode for 11 proteins (HA, NA, NP, M1, M2, NS1, NEP, PA, PB1, PB1, PB2).
- Because of the segmented nature of the genome when a cell is infected by two different viruses of a given type, mixtures of parental gene segments, may be assembled in progeny visions. This phenomenon call genetic re-assortment, may result in sudden changes in viral surface antigens- a property that explains the epidemiological features of influenza and poses significant problems for vaccine development.
- Also contains a viral RNA-dependent RNA polymerase that transcribes the negative polarity genome into mRNA.
- Three large proteins (PB1, PB2, and PA) are bound to the viral Ribonucleoprotein and are responsible for RNA transcription and replications.
- The matrix (M1) protein which forms a shell underneath the viral lipid envelope is important in particle morphogenesis and is a major competent of the virion.
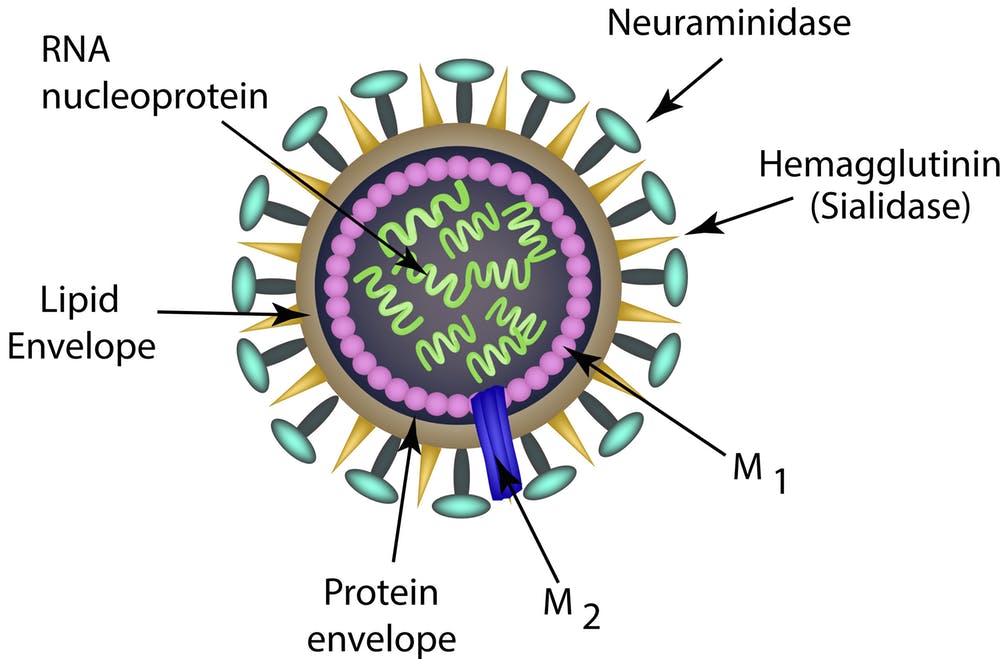
- Envelope and glycoprotein spikes:
- The nucleocappsid is surrounded by an envelope which has an inner membrane of protein known as matrix or M protein which is virus encoded and outer lipid layer derived from infected host cell membrane during the process of replication by budding.
- Two virus encoded glycoproteins, the haemagglutinin (HA) and the neuraminidase (NA) are inserted into the envelope and are exposed as spikes about 10mm long on the surface of the surface of the particles.
- These glycoproteins are triangular and mushroom shaped respectively. They are synthesized in the early period of replication cycle, and get attached to the plasma membrane at specialized patches where budding occurs.
- These two surface glycoproteins are the important antigens that determine antigenic variation of influenza viruses and host immunity.
- The HA represents about 25% of viral protein the NA about 5%.
- The M2 ion channel and the NS2 protein are also present in the envelope but a few copies per particle.
- Haemagglutinin (HA):
- Haemagglutin derives its name from its ability to agglutinate erythrocytes under certain conditions.
- Haemagglutinin is a glycoprotein composed of two polypeptides- HA 1 and HA2, responsible for hemadsorption and haemagglutination. These two polypeptides are joined together by disulfide bond.
- The Haemagglutinin consists of 500 spikes each measuring 12nm in length.
- The triangular shaped HA is inserted into the virus membrane by its tail end which is hydrophilic in nature. The distal end which contains five antigenic sites (HA1-HA5) is responsible for binding of vision to host cells.
- Haemagglutinin is one of the major antigen of influenza virus and is responsible for antigenic variation.
- HA enables the virus to absorb to muco-protein receptors on red cells as well as an respiratory epithelial cells.
- HA agglutinates certain RBCs which is inhibited by the neutralizing antibodies. This forms the basis of the haemagglutination inhibition test used in the sero-diagnosis of influenza.
- Neurominidase (NA):
- Neuraminidase is a glycoprotein receptor and is important in determining the subtype of influenza virus isolates.
- It consists of 100 mushroom-shaped spikes that is a tetramer, composed of four identical monomers. A slender stalk is tapped with a box shaped head.
- NA functions at the end of the viral replication cycle.
- Neuraminidase is a sialidase enzyme that removes sialic acid from glycol-conjugates. It causes hydrolysis of N-acetyl neuraminic acid or sialic acid residues present on the glycoprotein receptors on red cells, hence causes elution or detachment of cells absorbed to virion particles.
- It facilitates release of the virus particles from infected cells surface during the budding processes and helps prevent self-aggregation of virions by removing sialic acid residues from viral glycoprotains.
- It also degrades the mucus layer, thereby exposing the epithelial membrane of the respiratory tract for infection of the virus.
Types of Influenza viruses
On the basis of antigenic differences in nucleoprotein and the matrix protein (M) the influenza virus is divided into 3 types.
- Influenza virus A:
- They are the causative agent for all flu pandemics and are known to infect humans other mammals and birds.
- Influenza A virus are further classified into sub types based on the properties of their major membrane glycoproteins; Haemagglutinin and Neuraminidase.
- Till now, 15 HA (H1-H15) sub types and 9 NA1 (N1-N9) sub types have been identified from influenza viruses of birds, animals and humans.
- Influenza virus B1: They are known to infect humans and seals.
- Influenza virus C: They are known to infect humans and sometimes pigs.
Nomenclature and classification of Influenza virus:
- WHO in 1971 proposed a new system of classification and was later modified.
- According to this the complete designation of a strains will include the (a) type (b) place of origin (c) serial number and (d) year of isolation followed by (e) antigenic subtypes of the HA and NA in parentheses.
Antigenic variations:
One important characteristics of Influenza virus is that, it regularly change their surface antigen (haemagglutinin and neuraminidase present in the surface). These antigenic changes are of two types; antigenic shift and antigenic drift
- Antigenic shift
- It is the major and drastic and discontinuous type of change in the antigenic structure, resulting in a novel virus strain which is antigenically unrelated to the predecessor strains.
- The antigenic shift occurs due to major antigenic changes in HA or NA antigens and is caused by replacement of the gene for Haemagglutinin by one coding for a completely different amino acid sequence due to exchange of whole RNA segment.
- This is characterized by alteration of virtually all the antigenic sites of the HA.
- The antigenic shift occurs when two different strains of Influenza virus infect a single host cell.
- Antigenic drift
- It is the minor and gradual sequential change in antigenic structure.
- Antigenic drift refers to the minor antigenic changes in either the haemagglutinin or neuraminidase or both.
- The drift results from point mutations in the HA and NA genes.
- The antigenic drift is characterized by changes in certain epitopes in the HA, while others are being conserved.
Mode of transmission of Influenza:
- Influenza virus infection transmits through air borne route as well as through contaminated hands
- It spreads from person to person via respiratory secretions during the acts of sneezing and coughing
- It also transmits by contact with contaminated hands or surfaces.
Pathogenesis of Influenza virus:
- Influenza virus enters the body through upper respiratory tract, where the virus attaches to and infects the mucosal epithelial cells.
- Influenza virus have some defense mechanism to protect itself from removing from cough reflex. Similarly, the influenza virus has also mechanism to protect itself from neutralization by IgA antibody present in mucus lining of upper respiratory tract.
- Viruses attach to sialic acid receptors on epithelial cells by their haemagglutinin spike present on the viral envelope.
- Neuraminidase lowers the viscosity of the mucous film in the upper respiratory tract and promoting the spread of virus containing fluid to lower respiratory tract.
- After attachment on epithelial cell, virus enters into the cell and begins the replication cycle.
- Infection of mucosal cells results in cellular destruction and degradation of the superficial mucosa. The resulting edema and mononuclear cell infiltration of the involved areas are accompanied by symptoms including non-reproductive cough, sore throat and nasal discharge.
- By continuous replication, epithelial layer of respiratory tract is completely removed. Then many opportunistic normal flora penetrate through damaged epithelium causing opportunistic bacterial infections. Many bacteria like Eg. Streptococcus, staphylococcus and Haemophilus influenza are carried into lungs along with mucus. In lungs these bacteria multiply causing secondary bacterial pneumonia.
- Occasionally in patients with underlying heart or lung disease the infection may extensively involve the alveoli, resulting in interstitial pneumonia, sometimes with marked accumulations of edema and lung haemorrhage.
- Influenza virus remains localized in epithelium of upper respiratory tract and do not penetrate into inner tissues. So influenza virus is not found in blood of infected individuals.
Clinical manifestation of Influenza:
- Uncomplicated Influenza; Flu like symptoms
- Symptoms of classic influenza include chills, headache, dry cough followed by high fever, generalized muscular aches, malaise and anoxeria.
- Sneezing, rhinorrhea and nasal obstruction are common.
- Patients may also report photophobia, nausea, vomiting, diarrhoea.
- The fever usually last for 3-5 days.
- Respiratory symptoms typically last another 3-4 days.
- The cough and weakness may persists for 2-4 weeks after major symptoms subside.
- Clinical symptoms of influenza in children are similar to those adults although children may have fever and higher incidence of gastro intestinal manifestation such as vomiting.
- Pneumonia
- Serious complications of influenza usually occur in the elderly and immune-compromised individual especially those with underlying chronic disease.
- Pregnancy appears to be risk factor for lethal pulmonary complications in some epidemic.
- The lethal impact of influenza epidemic is reflected in the excess death due to pneumonia and cardiopulmonary disease.
- Pneumonia complicating influenza can be viral, secondary bacterial or a combination of two.
- Increased mucous secretion helps to carry the agents into the Lower respiratory tract. Influenza infection enhances the susceptibility of patients to bacterial infections.
- The major bacterial pathogen associated are S. aureus, S. pneumonia and H. influenza.
- Combined viral bacterial pneumonia is approx. 3 times common than primary influenza pneumonia.
- Reye’s syndrome
- Reye’s syndrome is an acute encephalopathy of children and adolescent usually between 2-16 years of age.
- The cause of Reye’s syndrome is unknown but it is a recognized rare complications of Influenza B and A.
- Guillain- Barre syndrome
- It is characterized by encephalomyelitis and polyneuritis which is a rare complication of influenza virus infection.
Laboratory diagnosis of Influenza virus
Sample:
- Samples for diagnosis includes- nasal or throat washing, throat swab, gargles which are collected within 3 days after infection or appearance of symptoms.
- If the sample is for isolation of virus, it should be kept at 4°C. if storage time is more than 5 days, sample should be frozen at -70°C.
- Serum sample is needed for serology to detect antibody.
Method of diagnosis of Influenza virus:
- Direct antigen detection
- Various antigens of virus can be detected in nasal washing and throat swab. Antigens are components of virus which are left during assembly of virus particles.
- Rapid diagnosis of influenza may be made by demonstration of the viral antigen directly by ELISA or Florescence antibody test (FAT) or Radio-immuno-assay (RIA), using specific monoclonal antibodies.
- Isolation and identification of virus
- Virus isolation is obtained readily from patients during the first two or three days of illness.
- Throat gargles is the best specimen and is collected in saline broth or a buffered salt solution and is sent immediately to the laboratory or if delayed, stored at -4 degree Celsius. Isolation can be made in eggs or in monkey cell culture.
- The specimen is inoculated into the amniotic cavity of 11-13 day old eggs.
- After incubation at 35 degree Celsius for 3 days, the amniotic fluid and allantoic fluids are harvested separately and tested for haemagglutinin. This is carried out by using fowl and guinea of red cells in parallel and incubating at room temperature at 4 degree Celsius.
- Usually Influenza A agglutinate only guinea pig cells, influenza B agglutinateboth fowl and guinea pig red cells and influenza C agglutinate only fowl cells at 4 degree Celsius.
- The isolate is identified and typed by Complement fixation (CF) test with antisera to types A, B and C.
- Subtype identification is made by Hemaggluination inhibition test.
- Inoculation into monkey kidney or baboon kidney is the preferred method where facilities are available. Inoculated cell cultures are incubated with or without serum and in presence of trypsin, virus growth in tissue cultures is detected by direct demonstration of viral antigen in infected cell cultures by Immunoflurescence or by testing for hemadosorption with human, fowl and guinea pig red cells. In a positive hemadsorption test, red cells adhere to the virus budding from infected cells. Now a days most laboratory uses secondary baboon kidney or Mardin- Darby canine, kidney (MDCK) cells.
- Serodiagnosis:
- Antibodies to several viral proteins (hemagglutinin, neuraminidase, nucleoprotein and matrix) are produced during infection with influenza virus.
- Routine serodiagnosis test in use are hemagglutination inhibition assay (HIA) and ELISA, FAT etc to detect antibodies.
- To confirm recent infection, two serum samples, one collected during acute phase and other during convalescence phase are needed. Four fold rise in antibody titer in acute phase is indication of recent infection.
- Molecular diagnosis:
- Rapid test based on detection of influenza RNA in clinical specimen using RT-PCR is also possible.
Treatment of Influenza virus:
- Two antiviral drugs- Amantadine and Rimantadine are available for treatment of influenza. These drugs are effective for type A but not against type B.
- Zanamivir and Oseltamivir are newer drugs for treatment of influenza and are effective against both influenza type A and B viruses.
- Vaccine: Due to antigenic shift and drift, vaccine production is difficult.
