Haematopoiesis
- Haematopoiesis is defined as the process of formation, development and differentiation of blood cells.
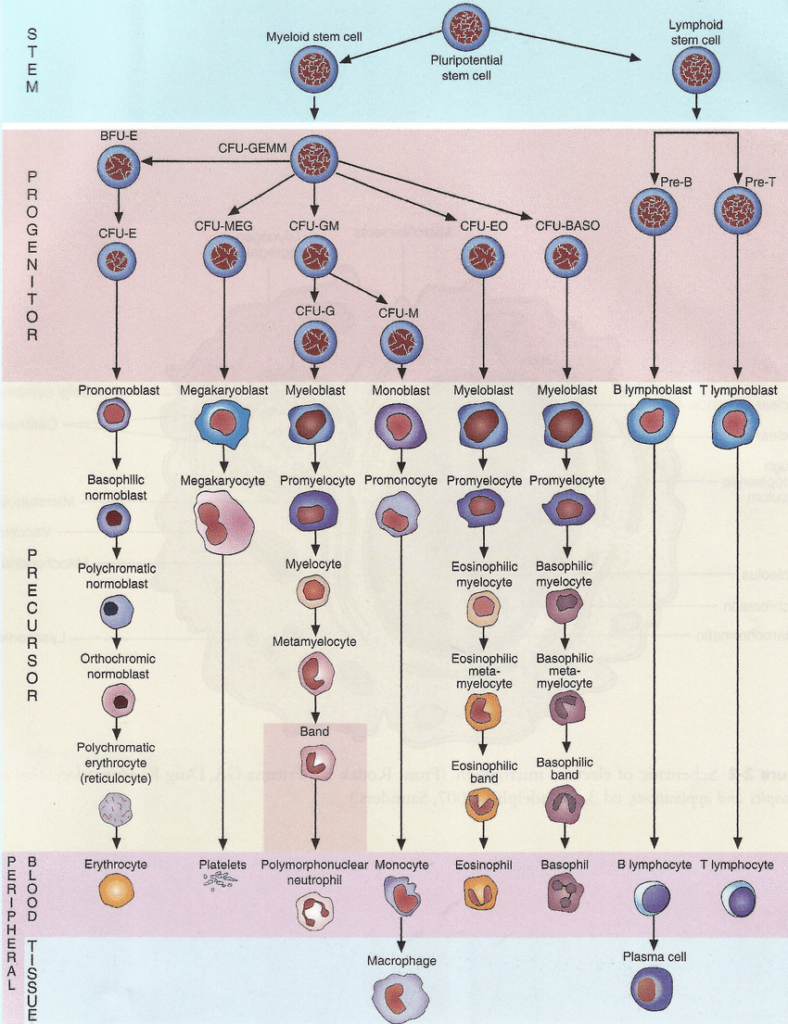
- The blood cells are formed from haematopoietic stem cells (HSCs) which are either multipotent or pluripotent in nature.
- In the prenatal stage, haematopoiesis occurs in the yolk sac during the first weeks of embryonic development and transitions to the spleen, liver, lymph nodes and finally in the bone marrow continuing for lifetime.
Hematopoietic stem cells (HSCs) and types
- Haematopoietic stem cells (HSCs) are special type of cell present in rar the bone marrow, they are rare and their numbers are strictly controlled by a balance of cell division, death, and differentiation.
- HSCs divide generating daughter cells. Some daughter cells retain the stem-cell characteristics of the mother cell having property of self self-renewing and able to give rise to all blood cell types. While other daughter cells differentiate into progenitor cell that lose their self-renewal capacity and giving rise to a particular blood cell lineage.
- Therefore, early in hematopoiesis, a multipotent stem cells differentiates along one of two pathways, giving rise to either a common lymphoid progenitor cells or a common myeloid progenitor cells
- Both the myeloid and lymphoid lineages are engaged in dendritic cell formation.
- Myeloid cells: It consists of-
- Monocytes
- Eosinophils
- Basophils
- Neutrophils
- Macrophages
- Erythrocytes
- Megakaryocytes
- Platelets.
- Lymphoid cells: It consists of-
- B cells
- T cells
- Natural killer cells
- Innate lymphoid cells.
The common myeloid progenitor cells:
- The common myeloid progenitor cell (CFU-GEMM) can differentiate into erythrocytes, thrombocytes, granulocytes, lymphocytes and monocytes.
- For the differentiation and proliferation of CFU-GEMM from HPCs, Interleukin-3 and Granulocyte-macrophage colony-stimulating factor (GM-CSF) are implicated.
- Stem cell factor (SCF) is a cytokine that can trigger the growth and total number of CFU-GEMM.
- CFU-GEMM is the precursor to several colony forming units which finally give rise to different blast cells.
- These consists of the following:
- CFU-Meg (from which promegakaryoblasts are produced)
- CFU-E (from which proerythroblasts are produced)
- CFU-GM (both monoblasts and myeloblasts are derived from this type of colony forming unit)
Process of hematopoiesis:
- According to the monophyletic theory of hematopoiesis, the pluripotent stem cells multiply to produce more of the pluripotent stem cells, making sure of the steady and lasting supply of stem cells.
- Some of the pluripotent stem cells now differentiate into precursor cells that are least partially dedicated to form one type of mature blood cell.
- Pluripotent cells multiply at low pace into one of the five possible unipotential stem cells.
- These unipotential stem cells then multiply rapidly into the precursor of the destined specific mature blood cell.
- The typical process of hematopoiesis consists of the differentiation of the multipotential hematopoietic stem cell into either the common myeloid or lymphoid progenitor.
- Then, relying upon the cytokines and resulting transcription factors that are activated, the myeloid progenitor can differentiate into a myeloblast.
- This myeloblast leads to granulocyte (basophils, eosinophils, or neutrophils) or monocyte (macrophages and dendritic cell) development.
- Also, it leads to the differentiation of megakaryocytes into platelets, or erythroblasts into erythrocytes.
- Lymphoid dendritic cells can form directly from the common lymphoid progenitor.
- Furthermore, the differentiation of the common lymphoid progenitor into a lymphoblast results the further development of natural killer cells or lymphocytes (T and B cells).
- Once B cells get activated in secondary lymphoid organs, it further differentiate into plasma cells.
- These plasma cells secrete antibodies.
Regulation of Haematopoiesis:
- Hematopoiesis is largely regulated by the presence of cytokines.
- These cytokines are responsible for regulating the differentiation of multipotential hematopoietic stem cells into specific cell types by the activation of transcription factors.
- The cytokines is very important for differentiation of particular cell types otherwise animal dies during embryogenesis.
- Some cytokines that regulates haematopoiesis are:
- Granulocyte macrophage-colony stimulating factor (GM-CSF):
- It enhances the myeloid lineage, finally leading to the differentiation of granulocytes and macrophages. Such cytokines are termed as growth factors.
- These growth factors are needed throughout the process of hematopoiesis functioning in order to activate transcription factors.
- Transcription factor GATA-2:
- It is required for the development of all hematopoietic lineages; in its absence animals die during embryogenesis.
- Transcriptional regulator Bmi-1:
- It is required for the self-renewal of HSCs, and in its absence animals die within 2 months of birth because of the failure to repopulate their red and white blood.
- Granulocyte macrophage-colony stimulating factor (GM-CSF):
- Other Examples of cytokines involved in haematopoiesis are:
- Colony-stimulating factors (CSFs)
- Erythropoietin (EPO)
- Thrombopoietin (TPO)
- Granulocyte colony-stimulating factor (G-CSF)
- Monocyte colony-stimulating factor (M-CSF)
- Tumor necrosis factor (TNF)
- Transforming growth factor (TGF)
- Stem cell factor (SCF)
- Leukemia inhibitory factor (LIF)
Erythropoiesis:
- The process of formation of red blood cells termed as erythrocytes is known as erythropoiesis.
- It is enhanced by decreased levels of oxygen in the blood, which signals for the secretion of erythropoietin.
- Erythropoietin is a hormone central to the formation of red blood cells.
- Erythropoiesis takes on average 2 days to be completed from to form mature red blood cell from unipotential hematopoietic cell.
- 2 million erythrocytes are produced every second in our bodies.
- Hematopoietic cells determined to become red blood cells usually get smaller and more condensed as they mature until there is finally loss of their nuclei.
- The unipotential cell becomes proerythroblast, which has uncondensed nucleus and has basophilic or blue cytoplasm.
- Then the cell becomes a basophilic erythroblast, which is followed by a polychromatophilic erythroblast stage.
- In polychromatophilic erythroblast stage, the nucleus becomes more condensed than the latter two stages and the cytoplasm is reduced.
- In the succeeding orthochromatophilic erythroblast stage, the nucleus is much smaller than that of the prior stages having a pinker cytoplasm.
- Then comes the reticulocyte stage, where the red blood cell lacks nucleus, but still stains somewhat blue because of the remnants of polyribosomes within the cell.
- Ultimately, the erythrocyte is the mature red blood cell, with no nucleus and no polyribosome remnants and as a result stains pink.
Granulopoiesis
- The process of formation of granulocytes is termed as granulopoiesis.
- Granulocytes are white blood cells having multi-lobular nuclei and cytoplasmic granules.
- The unipotential hematopoietic cell which forms a myeloblast is large.
- It has a cytoplasm that stains blue with a large nucleus.
- This cell gives rise into a promyelocyte that contains azurophilic granules. Then it becomes a myelocyte, which has a non-indented still rather large nucleus.
- This cell then gives rise to a metamyelocyte, which is alike in size to a mature granulocyte and the nucleus starts to become indented.
- After this stage is the band cell stage, where the nucleus resembles a horseshoe and has definitive indentation.
- Ultimately, there is the mature granulocytes having a lobed nucleus and cytoplasmic granules.
- The entire process occurs over a period of 2 weeks.
Monopoiesis:
- The process by which monocytes are formed is termed as monopoiesis.
- The monoblast is the committed progenitor cell, found only in the bone marrow. Also, monoblast has a basophilic cytoplasm without granules.
- These monoblasts give rise to promonocytes, which are smaller in size with nuclei that become slightly indented, before becoming monocytes.
- Monocytes have kidney-shaped nuclei and can develop into dendritic cells or macrophages.
Lymphopoiesis:
- The formation of lymphocytes, starts from their first committed progenitor cells, lymphoblasts, this process is called Lymphopoiesis.
- These cells after maturation, are able to differentiate into either B, T or natural killer cells.
Thrombopoiesis:
- Megakaryocytes, which are extremely large cells within the bone marrow forms the platelets, this process is termed as thrombopoiesis.
- When the plasma membranes of megakaryocytes are fragmented, the origin of individual platelets take place, thus generating platelets containing many granules.