Entamoeba histolytica: Morphology, life cycle, Pathogenesis, clinical manifestation, lab diagnosis and Treatment
- Entamoeba histolytica is a common protozoan parasite found in the large intestine of human. The parasite is responsible for amoebiasis and liver absceses. It is the third leading parasite cause of death in the developing countries.
Morphology:
- Parasite occurs in three stages; trophozoite, precyst and cyst
 1. Trophozoite:
1. Trophozoite:
- It is the growing and feeding stage of parasite
- Sape; not fixed because of constantly changing position
- Size: ranging from 18-40 µm; average being 20-30 µm
- Cytoplasm: cytoplasm is divided into two portion; a clear transparent ectoplasm and a granular endoplasm. Ingested RBCs, tissue granules and food materials are also found in endoplasm
- Nucleus: It is single, spherical shape and size ranging from 4-6µ Nucleus contains central karyosome and fine peripheral chromatin.
- Trophozoites are actively motile with the help of pseudopodia.
- Trophozoites are anaerobic parasite, ( present in large intestine)
2. Pre cyst:
- It is the intermediate stage between trophozoite and cyst
- It is smaller in size; 10-20µ
- It is round or slightly ovoid with blunt pseudopodium projecting from periphery
- No RBC or food materials are found on its endoplasm.
3. Cyst:
- It is the infective form of parasite.
- Shape: It is round or round or oval in shape
- Size: 12-15 µm in diameter
- It is surrounded by a highly retractile membrane called cyst wall. The cyst wall is resistant to digestion by gastric juice in human stomach
- Nucleus: A mature cyst is quadri-nucleated.
- Cytoplasm: Cytoplasm shows chromatid bars and glycogen masses but no RBCs or food particles.
- Mature cyst passed out in stool from infected patient and remained without fouther development in soil for few days.
Life cycle:
- Life cycle of histolytica is relatively simple and consists of infective cyst and invasive trophozoites stage.
- Life cycle completes in single host, ie human
- Human get infected with E. histolytica cyst from contaminated food and water. Infection can also acquired directly by ano-genital or oro-genital sexual contact.
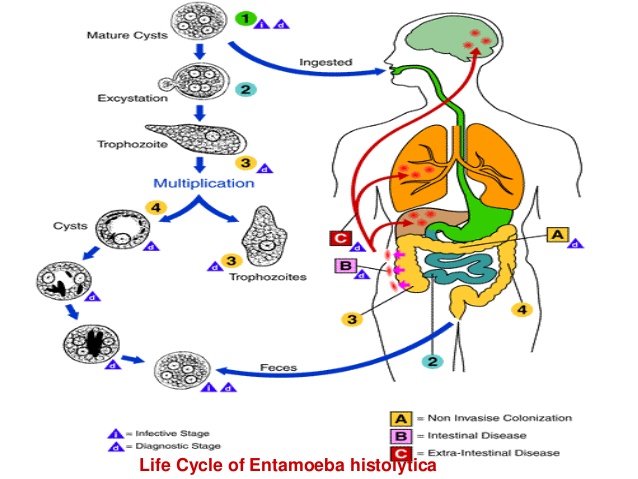
- The mature Cyst is resistant to low pH of stomach, so remain unaffected by the gastric juices.
- The cyst wall is then lysed by intestinal trypsin and when the cyst reaches the caecum or lower part of illium excystation occurs. The neutral or alkaline environment as well as bile components favor excystation.
- Excystation of a cyst gives 8 trophozoites. Trophozoites are actively and carried to large intestine by peristalsis of small intestine. Trophozoites then gain maturity and divide by binary fission.
- The trophozoies adhere to mucus lining of intestine by lectin and secretes proteolytic enzymes which causes tissue destruction and necrosis. Parasite, when gain access to blood, migrates and causes extra-intestinal diseases.
- When the load of trophozoites increases, some of the trophozoites stop multiplying and revert to cyst form by the process of encystation.
- These cysts are released in faeces completing the life cycle.
Pathogenesis:
1. Mode of infection:
- Faeco-oral route
- Ingestion of cyst contaminated foods and water
2. Virulence factors:
i. Cyst wall: cyst wall is resistant to low pH and gastric juice of stomach.
ii. Lectin: Surface of trophozoite contains lectin that is specific to lingards (N-acetyl-galactosamine and galactose sugar) present in surface of intestinal epithelium.
iii. Ionophore like protein: It causes leakage of ions such as Na+, K+, Ca++ from target cells.
iv. Hydrolytic enzymes: Phosphatase, proteinease, glycosidase and RNase causes tissue destruction and necrosis.
v. Toxin and haemolysin
3. Pathogenesis;
- The parasites express large number of virulence factors including lectin, lytic peptide, cysteine, proteineases and phospholipase.
- Excystation of cyst in intestine releases 4 trophozoites which then colonizes the large intestine. The binding of trophozoites with the colonic epithelium is a dynamic process in the pathogenesis. After adherence trophozoite lyse the target cell by its ionophore like protein that causes leakage of ions from cytoplasm. The proteolytic enzymes secreted by the amoeba causes tissue destruction giving flask shaped amoebic ulcer, is a typical feature of intestinal amoebiasis.
- Trophozoites penetrates the columnar epithelium of mucosa causing lysis and moves deep inside till they reached submucosa layer and multiply rapidly. Ultimately amoeba destroy considerable area of the submucosa leading an abscess formation which breaks down to form ulcer. The ulcer is flask shaped with narrow neck and broad base. The ulcer may be localized in ileo-caecal region or generalized throughout the large intestine.
- From intestine, the parasites may be carried to other vital organs such as liver, heart, brain etc through blood circulation. Pulmonary and hepatic amoebic abscesses are frequent and rarely cerebral, cutaneous and splenic amoebic abscesses.
Clinical manifestation:
- Infection ranges from asymptomatic to invasive intestinal amoebiasis and extra-intestinal amoebiasis
1. Intestinal Amoebiasis
i. Asymptomatic infection: 90% of E. histolytica infection is mild or asymptomatic
ii. Symptomatic infection
- Non dysentric amoeboic colitis (mild diarrhea)
- Acute amoebic dysentery: it is more common and characterized by abdominal pain, fever and tenderness. Stool contains RBCs, charcot-leyden crystals and trophozoites.
Complications: toxic megacolon, fulminant amoebic colitis, amoeboma, amoebic peritonitis, perianal ulceration
2. Extra intestinal amoebiasis:
i. Hepatic infection: non supurative hepatitis, liver abscesses, other complications
ii. Pulmonary infection: chest pain, dyspnoea, non-productive cough
iii. Cerebral infection: it is rare and occurs as a complication of liver of pulmonary amoebiasis
iv. Genitourinary infection: involves kidney and genital organs
v. Spleenic infection
vi. Cutaneous amoebiasis
- Amoebic pericarditis
Lab Diagnosis:
- Specimen: stool, pus or liver abscesses, sputum and biopsy samples
- i. Stool macroscopy: in amoebic dysentery stool is offensive, semi-solid, dark brown color and acidic in nature, mixed with blood, mucus and faecal materials.
- ii. Microscopy: Normal saline preparation of fresh faecal material revels trophozoites with RBCs in its cytoplasm and its amoebic motility.
- iii. Stool Ag detection: ELISA to detect 170KD lectin of E. histolytica
- iv. Stool culture: Robinson’s medium and NH polyxenic culture medium are used to culture E. histolytica
- v. Serology: IHA, IFA etc are used to detect antibody in serum against E. histolytica
- vi. PCR: It is sensitive test , used to differentiate E. histolytica with other Entamoeba species
- vii. Radiological finding: X-rays, MRI, CT scan, ultrasonography etc for extra intestinal amoebiasis..
- viii. Blood test: blood count, Liver function test, Kidney function test
- ix. Intradermal test
Treatment and prophylaxis:
- Diloxanide fluorate, diidohydroxyquin, paramycin, metronidazole, imidazole
- 4-aminoquinoline; for extra intestinal infection
- Oral rehydration
