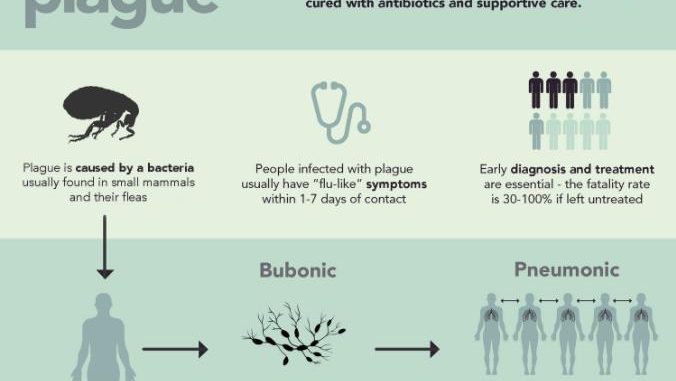
Transmission of plague:
- Plague is a zoonotic infection transmitted to human by the bite of an infected rat flea.
- Infection may also be transferred by contamination of the wound resulted by bite with the feces of infected rat fleas.
- Human to human transmission occurs only in pneumonic plague which is spread by droplet infection.
Pathogenesis of plague:
- Yersinia pestis is a highly virulent bacterium which causes plague with a high mortality rate. The ability of Yersinia spp. to resist pathogenetic killing is the hallmark of pathogenesis of plague.
- Y. pestis causes natural disease of rats and other rodents.
- The infected host dies. If no other rodent is available for the flea to colonize the flea searching for a new host transmit the infection to humans.
- In human plague occurs in 3 forms:
1. Bubonic plague:
- It is a zoonotic disease transmitted by rat flea Xenopsylla cheopsis from animals to humans.
- The fleas acquire the infection from infected rodents during biting. When rat fleas bite an infected or diseased rat, it sucks nearly 0.5 ml blood per fed containing nearly 5000-50000 plague bacilli.
- In the stomach of flea, the bacilli multiply rapidly blocking the proventriculus (region of stomach) and thereby prevent food entry into the stomach.
- The interval between the ingestion of infected blood and blocking in the proventriculus varies from 2 to 3 weeks in X. cheopis. It is known as extrinsic incubation period.
- When such infected flea bites other rodent it cannot suck in blood because the bacterium mass blocks the passage mechanically.
- Therefore, blood mixed with the bacteria is regurgitated during bite, transmitting the infection to the rodent.
- When the disease rat dies, the flea leaves the carcass and in the absence of another rat, bites human causing bubonic plague.
- The disease in humans occurs following the bite of rat flea, depositing thousands of bacilli into the host skin during blood meals.
- The bacilli then migrate to the regional lymph nodes, where they are phagocytosed by the PMNS and mononuclear phagocytes and multiply intracellularly.
- The phagocytosed bacilli are carried to lymphoid tissue, and causes characteristic inflammation, necrosis and hemorrhagic lymph node known as bubo, as demonstrated on bubonic plague.
- Infected lymph node shows large number of plague bacilli destruction of the normal architecture and medullary necrosis.
- Subsequent spread of bacteria occurs along the lymphatic channels towards the thoracic duct with external distribution of the bacteria in circulation leading to bacteremia and septicemia.
- The bacteria potentially infect every organ, including the lungs liver spleen, kidney and rarely even the meninges.
- Clinical symptoms of Bubonic plague:
- Bubonic plague is the most common clinical form of the disease.
- The incubation period varies for 2 to 6 days.
- Characteristic manifestation of bubonic plague are-presence of painful, swollen lymph glands usually in the grin, axilla and neck.
- The clinical manifestation is associated with a sudden onset of high fever, chills and headache and also body aches, extreme exhaustion, abdominal pain and diarrhea.
- Enlargement of buboes may cause rupture and discharge of foul- smelling pus.
- If untreated mortality rate is 40-70 %.
2. Pneumonic plague:
- It occurs by droplet infection with Y. pestis being passed from person to person, following direct inhalation of the bacilli by droplet infection due to close contact with infected host or by inhalation of aerosolized bacteria, such as may occur if used as a biological weapon.
- The bacilli spread through the lungs producing a severe and rapidly progressive multi-lobar bronchopneumonia, subsequently leading to bacteremia and septicemia.
- Clinical symptoms of pneumonic plague:
- Abrupt onset of fever and chills, lymphadenopathy, chest pain, dyspnea, purulent sputum or hemoptysis are the manifestation of pneumonic plague.
- If untreated, the condition is highly fatal.
3. Septicemic plague:
- When the plague bacilli are deposited directly in the circulation, bypassing the lymphatics, it caused primary septicemic plague.
- In such case, early dissemination of bacilli occurs but without the formation of a bubo.
- This is usually observed in the individuals bitten by the rat flea in the oral and pharyngeal area due to the vascularity of the tissue and short lymphatic distance to the thoracic duct.
- Clinical symptoms of septicemic plague:
- This may occur as a primary infection but it is usually secondary as the terminal event of bubonic and pneumonic plague.
- The condition is associated with rapid onset of symptoms such as nausea, vomiting, abdominal pain and diarrhea.
- Due to overwhelming infection, patients have a toxic appearance and may present with tachycardia, tachypnea, and hypotension.
- Generalized purpura leading to neurosis and gangrene of distal extremities may be observed.
- Buboes are not seen.
- Septicemic plague is associated with a high mortality rate and patients usually die due to high level of bacteremia.
- Pestis minor or benign plague is also seen. It is presented by a slight temperature with one or two swollen glands. Many show elevated antibody titers in serum.
Laboratory diagnosis:
Specimens:
- Bubo aspirates (bubonic plague), sputum and cerebrospinal fluid and blood in septicemic plague.
- Other specimens include throat swab or washing, skin swabs and scrapings.
- Specimens should be marked ‘High Risk’.
Microscopy:
- The specimen stained with Gram, Giemsa, Wright, Wayson stain for demonstration of the typical bipolar morphology of Y. pestis.
- Gram staining shows small, non-motile, Gram negative coccobacilli.
- Microscopic examination of buffy coat smear of peripheral blood may show Y. pestis in septicemic cases.
Rapid diagnosis:
- A direct fluorescent antibody test employing monoclonal antibodies is a rapid diagnostic method to demonstrate Y. pestis F1 antigen in blood or sputum samples.
- A positive fluorescent antibody test on cultures is presumptive evidence of infection.
Culture:
- Y. pestis is aerobic and facultatively anerobic.
- It grows at a temperature range of 2-45 °C with an optimum temperature of 27°C.
- The bacteria grows at a wide range of pH (5-9.6 with an optimum pH of 7.2).
- Y. pestis is a slow grower but it does not require any special growth media.
- For selective isolation of Y. pestis from sputum and bubo aspirates containing numerous other bacteria, Blood agar with sodium azide is used.
- On Nutrient Agar, colonies are small delicate, transparent that becomes opaque on prolonged incubation.
- On Blood Agar, colonies are dark brown due to absorption of the hemin pigment- non hemolytic colonies.
- On MacConkey Agar, colonies are non-lactose fermenters, growing best at 22-28° C. But colonies tend to auto-lyse after 2-3 days.
- On liquid media:
- Y. pestis produces a fluorescent growth with little or no turbidity. Granular deposit occurs at the bottom and along the sides of the tube.
- On prolonged incubation, a delicate pellicle may form at the surface
- Y. pestis produces a characteristics growth when grown in a flask of broth with oil or ghee floated on the top (ghee broth).
- The growth in the medium appears to hang down into the broth from the surface resembling stalactites (stalactite growth).
Bio chemical tests:
- Catalase: positive
- Oxidase: negative
- Coagulase: positive
- Indole: negative
- MR: positive
- VP: negative
- Citrate: negative
- Urease: negative
- Gelatin hydrolysis: negative
- Lysine decarboxylase: negative
- Phenylalanine deaminase: negative
- Ferments glucose, maltose and mannitol with production of acid but no gas.
- Lactose, sucrose, rhamnose: not fermented
- Nitrate reduction: negative
- Esculin hydrolysis: positive
- Growth in KCN medium: sensitive
Animal inoculation:
- The bubo aspirate is injected subcutaneously into the animal, death of the animal occurs within 2-5 days.
- Postmortem of the dead animal shows edema and necrosis at congested and shows grayish white patches.
- Sputum collected from suspected cases of pneumonic plague is inoculated by applying them over the shaven skin or to the nasal mucosa of guinea pig.
- The bacteria present in the specimen penetrates the skin through minute abrasions.
- Bacilli are demonstrated in the sputum and in the blood from the heart of guinea pig which dies 2-3 days after inoculation.
Serodiagnosis:
- Immunofluorescence and ELISA test detect F1 glycoprotein Ag-complex in serum or aspired fluid from bubo
- ELISA and indirect hemagglutination test are also employed to detect specific antibodies in acute and convalescent sera.
- A fourfold rise in antibody titer between acute and convalescent sera collected 10 days apart, demonstrated by ELISA or IHA test suggest plague infection.
Treatment:
- Tetracycline is the drug of choice
- Streptomycin, chloramphenicol, gentamicin, trimethoprim, ciprofloxacin and kanamycin are also effective.
Prevention and control:
- Identifying the source of infection is the key component in preventing outbreaks of plague.
- General preventive measures include reduction of the rat population by rodenticides and eradication of rat fleas from the rats.
- Liberal use of insecticide (DDT) to rat runs.
Vaccination:
Killed vaccine:
- Killed vaccine is widely used for active immunization.
- It is a whole bacterial culture antigen of a virulent strain of plague bacillus.
- A virulent strain of the plague bacillus is grown in Casein hydrolysate broth for 2-4 weeks at 32° C and killed by 0.05% formaldehyde and preserved with phenyl mercuric nitrate.
- The vaccine is given subcutaneously, 2 doses at an interval of 2-3 months followed by a third six month later.
- This killed vaccine have some protection against bubonic plague but not against pneumonic plague. Also, the protection does not last for more than 6 months.
Live vaccine:
- Live vaccines are prepared from two avirulent strain of Y. pestis, Otten’s Tjiwidej strain from Jawa and Girard’s EV 76 strain from Malagasey.
- The vaccines have been found to confer much greater protection in animals than killed vaccine but because of difficulty of their preparations, mass immunization is not possible.
Epidemiology of plague:
- Plague is zoonotic disease and Humans are the accidental hosts.
- Epidemiologically there are two natural cycles of plague, the urban plague and the wild plague.
The urban plague:
- Urban plague is maintained in rat population and is transmitted among rats or between rats and humans by infected rat fleas.
- Domestic rat is the important reservoir of urban plague from which the infection spreads to human beings.
- The rat flea is the usual vector.
- 30 different flea species have been identified as vectors, the most important being Y. cheopis, X. astia and Ceratophyllus fasciatus.
- X. cheopis is the predominant one.
Wild or sylvatic plague:
- This occurs between animals and wild rodents independent of human beings.
- Different animal species have been identified as hosts such as domestic cats and dogs, squirrels, camels and sheep.
- A sylvatic stage occurs when humans are infected from these wild animals.
- Human infection may occur during handling of dead carcasses of infected wild animals and through the ingestion of meat of infected animals.
- Human infection from inhalation of respiratory droplets from infected cats has also been documented.