Visceral leishmaniasis (VL) or Kala-azar:
- Visceral Leishmaniasis (VL) also known as kala-azar or black fever or dum-dum fever, is the most severe form of leishmaniasis.
- The parasite migrates to the internal organs such as liver, spleen and bone marrow, and if left untreated it will almost always result in death of the host.
- The incubation period of the disease generally varies from 2 to 6 months but it may exceed 1-2 year.
- Young malnourished children are most susceptible to the development of progressive infection.
- Symptoms:
- Pyrexia:
- Itis often an early symptom and it may be continuous or remittent in type
- Waves of pyrexia may be followed by apyrexial period.
- Fever may be accompanied by sweating with chills but rigor. However, malaise is unusual.
- Splenomegaly:
- Splenic enlargement is one of the most striking features and the organ progressively enlarges.
- The abdomen is protuberant because of the splenomegaly and the accompanying hepatomegaly.
- With progress of the disease, the spleen extends to well below costal margin.
- The spleen is usually firm to hard but soft spleen can be seen in acute disease.
- Jaundice:
- Jaundice with mildly elevated enzyme levels is rarely seen and considered a bad prognostic sign.
- Lymphadenopathy:
- It is observed in the African and Chinese forms but is rarely observed in Indian forms.
- Hepatomegaly:
- Liver is enlarged but less conspicuous.
- It is soft with a smooth surface and a sharp edge.
- Kupffer cells greatly increase in size and number.
- The sinusoidal capillaries are dilated and engaged with blood.
- – There is a slight increase of reticulin fibrils developing as a result of Reticule endothelial proliferation.
- Anemia:
- It is almost always present and is usually severe.
- The anemia is normochromic and normocytic type, caused by various factors including replacement of marrow by the parasites, splenic sequestration, hemorrhage, hemodilution and hemolysis.
- Leukopenia and thrombocytopenia:
- Leukopenia is also observed and may contribute to secondary infection.
- Thrombocytopenia contributes to hemorrhagic tendency observed in some cases.
- Black fever:
- With the progress of the disease the skin becomes dry, thin and scaly and hair is lost.
- The skin on the hands, feet, abdomen and face may become darkened which is why the disease is also termed as kala-azar or black fever.
- Petechiae and ecchymosis may be seen in the extremities.
- Skin lesions that contains parasites and appear as diffuse, warty, nonulcerative lesions may occur in visceral leishmaniasis, especially in Africa.
- Mucosal lesions in the mouth and nose which appear as nodules or ulcers and may lead to perforation of the nasal spectrum, have been described in Sudan but are rare elsewhere.
- Hypergammaglobulinemia immune complexes and RF are present in sera of most patients of VL> rarely immune complex deposition in the kidneys may lead to mild glomerulonephritis.
- If untreated, death occurs within 2 years.
Post kala-azar Dermal Leishmaniasis (PKDL)
- PKDL occurs after treatment of VL in approx. 10 % of cases in India and 2 % cases in Africa.
- It is characterized by the formation of dermal lesions.
- These lesions are categorized in 3 types:
- Defragmented macules are earliest and are spread on the trunk and extremities.
- Erythematous patches appear early in the course of disease and are seen on the nose, cheeks and chin with a butterfly distribution. They are photosensitive and becomes prominent towards the middle of the day.
- Yellowish pink nodules appear mostly on the face and replace the earlier lesions.
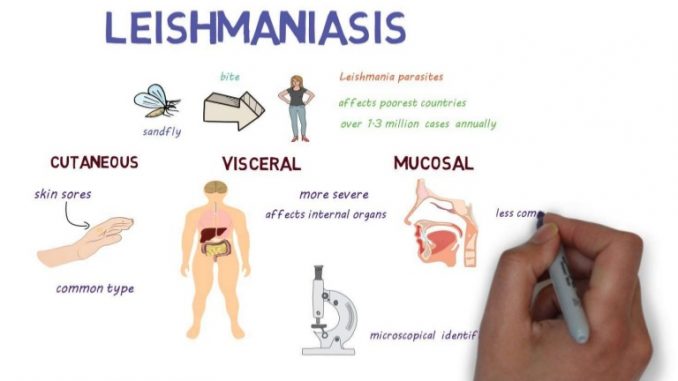
Cutaneous leishmaniasis (CL):
- It occurs in 2 forms:
- An oriental sore caused by L. tropical.
- American cutaneous leishmaniasis caused by L. braziliensis.
- Cutaneous leishmaniasis is characterized by lesions
- Lesions may be ulcers, smooth nodules, flat plagues or hyperkeratotic waste.
- The initial lesions occur in the skin that was exposed to sand flies and remain localized.
- However, in some cases the parasites may spread via the lymphatic to produce secondary lesions on the skins or occasionally the mucosa of other parts of the body.
- Regional lymphadenopathy sometimes occurs.
- Most skin lesions heal spontaneously
- Disseminated leishmaniasis is a rare form of cutaneous leishmaniasis. Especially L. amazonesis caused disseminated infection.
- The nodules do not ulcerate but they spread widely on the skin.
- They may cause damage to deep tissues and can persist indefinitely.
- The diffuse form can be incurable in some cases.
Lupoid leishmaniasis:
- It is a rare form of leishmaniasis.
- It is characterized by the spread of new lesions around the edges of a healed skin lesion.
- It is caused by L. tropica or L. braziliensis
- Lesion does not heal without treatment.
Mucocutaneous leishmaniasis:
- It is also known as espundia
- This form of leishmaniasis usually occurs in Latin America caused by L. braziliensis and less often by L. canariensis/ L. guyanensis.
- It is characterized by erythema and ulceration followed by destructive inflammation that can spread nasal septum, in some cases the pharynx and larynx.
- Frequent nosebleeds is an early sign.
- The inflammation can perforate the nasal septum, causes severe disfigurement of the face or block the pharynx or larynx.
- In some case the genitalia may also be involved.
- The lesion does not heal spontaneously.
Epidemiology and geographical distribution:
- Leishmaniasis is found in 88 countries and in 5 continents except Australia and Antarctica.
- Annual incidence of the disease is 600000 cases per year.
- An estimated 12 million people are infected worldwide and 350 million people are at risk of these approx. 25 % are of VL.
- Leishmaniasis is found worldwide.
- Most of the affected countries are in the tropics and sub tropics.
- More than 90% of the world cases of VL are in India, Bangladesh, Nepal, Sudan and Brazil.
Leishmaniasis in Nepal:
- VL is common in terai region.
- First confirmed case of VL was recorded in 1980.
- A total of 25890 cases with 599 deaths were reported during 1980-2006.
- During 2003, highest incidence (1 per 100000) was in Mahottari.
- Highest case fatality rate was in Dhanusha district 2.9% followed by Bara 2.4 % CL is rare in Nepal.
- First case of CL was reported in year 2006 in Nepal.
