Laboratory diagnosis of malarial parasite:
1. Specimen: blood
- Blood is collected from finger tips or ear lobe in older children and adults. In case of infants blood is collected from great toe.
- Smear should be examined atleast twice daily until parasite is detected.
2. Methods of examination:
i. Light microscopy:
- After blood collected from capillary, smear is prepared and stained with Romanwsky’s stain.
- Thick smear is used for detecting the parasite, quantitating parasitaemia, demonstrating malarial pigments.
- Thin smear is used for detecting parasites and also for determining the species.
- Diagnostic of falciparum is
- –detection of multiple rings in a single RBC with accole form
- Presence of maurer’s dots in RBC containing large ring
- Presence of characteristics banana shaped gametocyte
ii. Fluorescence microscopy:
- Kawanoto technique is a fluorescent staining method for demonstrating malarial parasites.
- In this method, blood smears are prepared on a slide and are stained with acridine orange. This is a differential staining. Nuclear DNA stained green and cytoplasmic RNA stained red.
- The stained slide is examined with fluorescence microscope for identification of parasite.
iii. Quantitative buffy coat (QBC):
- This is a sensitive method for detection of malarial parasite.
- It is based on the ability of acridine orange to stain nucleic acid of parasite.
- In this method, blood is collected in a capillary tube coated with fluorescent dye and is subjected to microhaematocrit centrifugation in a specialized centifuse.
- After centrifugation the buffy coat in the tube is examined directly under a fluorescence microscope. Parasite appear brilliant green.
- QBC is more sensitive than thick smear preparation.
iv. Serology:
- IHA, IFA and ELISA
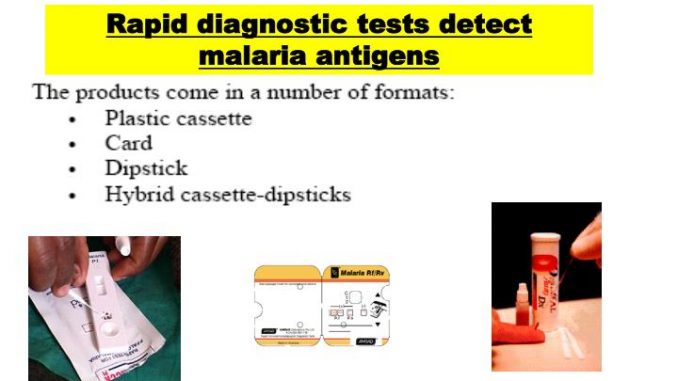
v. Dipstick test:
- It is a rapid diagnostic test extremely useful for rapid diagnosis of cerebral malaria.
- This is an enzyme immunoassay which detects histidine rich protein 2 (pf HRP-2) antigen, a metabolic product specifically produced by falciparum.
- Monoclonal antibodies produced against pfHRO-2 antigen is employed in the test to detect antigen in serum or urine.
- Dipstick test is only useful for detecting falciparum
vi. Molecular diagnosis:
- DNA probe is high;y sensitive. It can detect even a low parasitaemia (<10 parasite/ µl of blood). It is useful to detect drug resistant parasites.
- PCR is highly sensitive and can detect a single P. falciparum in 20µl of blood using PBRK1 primer.
- PCR can be used for identification of malarial parasite
vii. Biochemical diagnosis:
- A normochromic, normocytic haemolytic anaemia
- Leucopenia
- High Erythrocyte sedimentation rate
- Prolonged prothrombin and partial thromboplastin time in severe infection
- Normal plasma concentration of electrolytes, blood and urea nitrogen in uncomplicated malaria
- Decreased anti-thrombin II levels is mild infection
- Metabolic acidosis
- Hypergamma-globulinaemia
- Normal urine analysis
- Biological false positive reaction with VDRL test
