Microorganisms found on the skin
- The normal flora are regularly distributed among specific areas of our body and are extremely complex including of more than 200 species of bacteria. The composition of the normal flora is determined by various factors, including age, sex, genetics, stress, nutrition, and environmental factors as such pH, oxygen, concentration, moisture content, and types of secretions related with the anatomical site. It has been estimated that a human adult is a home to about 1012 bacteria on the skin, 1010 in the mouth, and 1014 in the gastrointestinal tract.
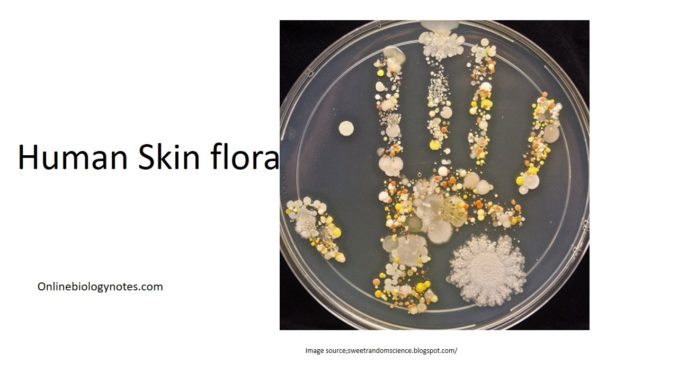
- Normal Flora of the Skin:
The adult human is wrapped up with approximately 2 square meters of skin. The density and make-up of the normal flora of the skin differs with anatomical locale. The skin microbes present in the most peripheral layers of the epidermis and the upper parts of the hair follicles are Gram-positive cocci (Staphylococcus epidermidis and Micrococcus sp.) and corynebacteria such as Propionibacterium sp. These are normally non-pathogenic and regarded as commensal, although mutualistic and parasitic roles have been allotted to them. The individuals who are nasal carriers, carry potentially pathogenic Staphylococcus aureus on their hands and face. It is because the face and hands are likely to become inoculated with the bacteria on the nasal membranes. - Normal Flora of the Conjunctiva:
A number of bacteria may be cultured from the normal conjunctiva, but the number of organisms is usually less. Staphylococcus epidermidis and certain coryneforms (Propionibacterium acnes) are majorly present. Staphylococcus aureus, some streptococci, Haemophilus sp. and Neisseria sp. are occasionally found. The continuous secretions from the lachrymal glands keeps the conjunctiva moist and healthy. - Normal Flora of the Respiratory Tract:
- The upper respiratory tract (nasopharynx) is colonized by a large number of bacterial species. The nostrils are always densely populated, mostly with Staphylococcus epidermidis and corynebacteria, and rarely (in about 20% of the general population) with Staphylococcus aureus. The healthy sinuses are sterile. The pharynx (throat) is generally colonized by streptococci and various Gram-negative cocci. Pathogens such as Streptococcus pneumoniae, Streptococcus pyogenes, Haemophilus influenzae and Neisseria meningitidis colonize the pharynx sometimes.
- Normal Flora of the Urogenital Tract:
- Urine is generally sterile, and since the urinary tract is drived with urine every few hours, microorganisms have difficulty in gaining access and to form colonies. The anterior urethra, may be colonized by a relatively persistent normal flora including of Staphylococcus epidermidis, Enterococcus faecalis and some alpha-haemolytic streptococci as per indicated by urine cultures. Their numbers are insufficient, however. In addition, some enteric bacteria (e.g. E. coli, Proteus) and corynebacteria, may occasionally be present at the anterior urethra.The vagina becomes colonized soon after birth with corynebacteria, staphylococci, streptococci, E. coli, and a lactic acid bacterium historically named “Doderlein’s bacillus” (Lactobacillus acidophilus).
- Normal Flora of the Oral Cavity:
- Mouth becomes a favourable habitat for various bacteria due to the presence of nutrients, epithelial debris, and secretions. Oral bacteria consists of streptococci, lactobacilli, staphylococci and corynebacteria, with a large number of anaerobes, especially bacteroides.
- Normal Flora of the Gastrointestinal Tract:
The bacterial flora of the gastrointestinal (GI) tract of animals has been studied more broadly than that of any other site. The composition varies between various animal species, and among the animal species. In humans, there are variations in the make-up of the flora which are affected by age, diet, cultural conditions, and the use of antibiotics. The latter greatly disturbs the composition of the intestinal flora. The proximal small intestine has a relatively less Gram-positive flora, consisting mainly of lactobacilli and Enterococcus faecalis. This region has about 105 – 107 bacteria per ml of fluid. The distal part of the small intestine includes greater numbers of bacteria (108/ml) and additional species, including coliforms (E. coli and relatives) and Bacteroides, in addition to lactobacilli and enterococci. In the upper intestine, mostly lactobacilli and enterococci are present. In the lower intestine and colon, 96% to 99% is constituted of anaerobes such as members of the genera Bacteroides, Lactobacillus, Clostridium, and Streptococcus, and 1% to 4% is made up of aerobes, including coliforms, enterococci, and a small number of Proteus, Pseudomonas, and Candida species.
Requirements for isolation of skin flora:
- Media:
- Blood agar
- Mannitol salt agar
- Chocolate agar
- Mueller-Hinton tellurite or Tinsdale agar
- Sabouraud agar plate
– two 5-ml sterile saline tubes.
- Reagents:
- Crystal violet
- Gram’s iodine
- Safranin
- 1% p-aminodimethylaniline oxalate
- lactophenol–cotton-blue.
- Equipment:
– Sterile cotton swabs
– tongue depressors
– desiccator jar with candle
– microscope
– glass slides
– Bunsen burner
– glassware marking pencil
– disposable gloves.
Procedure for isolation of skin flora
- Specimen from mouth:
- Place a tongue depressor on the extended tongue and with a sterile cotton swab, obtain a specimen from the palatine tonsil by rotating the swab vigorously over its surface without touching the tongue.
- Inoculate the swab in a tube of sterile saline and mix until uniform suspension is obtained.
- Using a sterile inoculating loop, inoculate one plate each of blood agar, chocolate agar, mannitol salt agar, and Mueller-Hinton tellurite or Tinsdale agar, all previously labelled with the source of the specimen, by means of a four-way streak inoculation.
- Specimen from skin:
- Using a sterile cotton swab moistened in sterile saline, obtain a specimen from the skin by rubbing the swab vigorously against the palm of the hand.
- Inoculate a tube of sterile saline with the swab and mix the solution.
- Inoculate one plate each of blood agar, mannitol salt agar, and Sabouraud agar.
- Incubate the inverted chocolate agar plate in a CO2 incubator, in a CO2 incubation bag, or in a candle jar for 48 hours at 37°C.
- For the fastidious organism like Neisseria 5% to 10% CO2 environment is required
- Incubate the inverted Sabouraud agar plate for 48 hours at 25°C.
- Incubates the remaining culture plates of blood agar, mannitoal agar, for 48 hours at 37°C.
Staining and Morphological Characteristics
- Prepare two Gram-stained smears from each of the blood agar cultures, choosing well-isolated colonies that differ in their cultural appearances and demonstrate haemolytic activity.
- Observe microscopically for the Gram reaction and the size, shape, and arrangement of the cells.
- Record the observations in the Lab Report and attempt to identify each isolate.
- Prepare two lactophenol–cotton-blue–stained smears of organisms obtained from discrete colonies that differ in appearance on the Sabouraud agar culture.
- Observe microscopically, draw a representative field in the Lab Report, and attempt to identify the fungi.
Observation and results:
- Examine the blood agar plate cultures for zones of haemolysis,
- Add the p-aminodimethylaniline oxalate to the surface of the growth on the chocolate agar plate. Observe for the appearance of a pink to purple to black colour on the surface of any of the colonies.
- Examine the Mueller-Hinton tellurite or Tinsdale agar plate for the presence of black colonies.
- Examine the Sabouraud agar plate for the appearance of moldlike growth.
- Examine the mannitol salt agar plate for the presence of growth that is indicative of staphylococci. Then examine the colour of the medium surrounding the growth. A yellow colour is indicative of S. aureus.
- Record your observations in the Lab Report and indicate the types of organisms that may be present in each specimen.
