Hepatitis B virus
- Hepatitis B is the most widespread and most important type of viral hepatitis. Hepatitis B virus (HBV) infects the liver and to less extent kidney and pancreas.
- It belongs to Hepadna viridiae family
- Mammalian hepadna virus consists of outermost surface antigen (HBsAg) which has 240 units.
- It is ds DNA virus. However one of the strand is shorter than another strand
- It has circular DNA
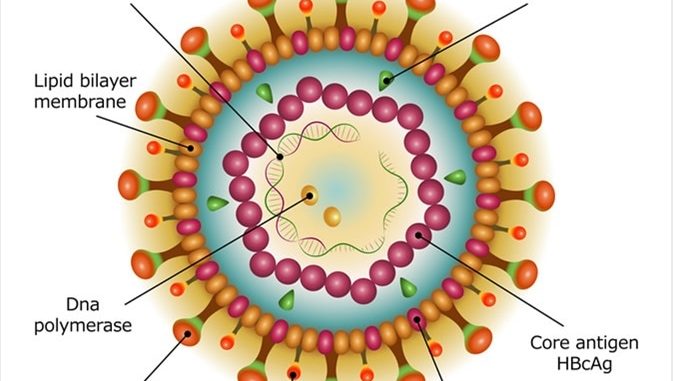
Structure of Hepatitis B virus:
- HBV is a small, enveloped DNA virus measuring 42 nm in diameter. It has an outer envelope and an inner core which is 27 nm in diameter enclosing the viral genome and a DNA polymerase.
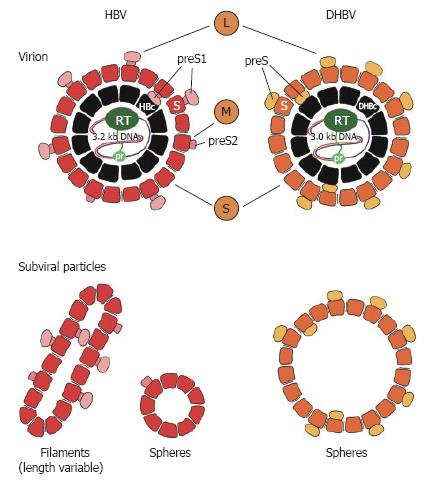
- Three types of morphological form can be seen;
- Small 20-22nm circular or spherical form: this is the most abundant form and it comprises of viral surface proteins.
- 20 x 200 nm filamentous form known as Australia antigen
- Double walled 42nm spherical form called Dane particle: this particle is the complete hepatitis B virus.
- Envelope consists of at least three membrane spanning proteins;
- Large Hepatitis B virus surface (LHBS) protein: LHBS consists of S-domain as well as pre-S-domain (pre-S1 and pre-S2), both internally and externally. LHBS is important for infection.
- Medium hepatitis B virus surface (MHBS) protein: MHBS is made up of S-domain and pre-S2 domain
- Small hepatitis B virus (SHBS) protein: SHBS consists of only S-domain. It is the main constituent of virus envelope and is important for virion assembly
Antigen present in Hepatitis B virus:
- There are different types of group specific surface antigen (HBs Ag). The most common group of surface antigen of all Hepatitis B virus is ‘a’ with two other antigenic soft determinants d/y or w/r. combination of these antigens resulting in four different strains- (adw, adr, ayr or ayw). Among these strains adw is most common.
- There are two glycosylation sites resulting in at least 6 different types of surface proteins. They are GP-42, GP-39, GP-36, GP-33, GP-27, and GP-24)
- Surface antigen (HBs Ag) encircles 25-28nm core.
- The core antigen is made up of nucleo-capsid which consists of DNA and capsid (HBc Ag)
- Surface antigen interacts with the core antigen with the help of heat shock protein 70 (hsc70).
- The core encapsidate the viral DNA and the enzyme DNA polymerase.
- DNA polymerase consists of 4-domains
- Priming domain
- Tetner (spacer) domain
- Reverse transcriptase domain to transcribe RNA into DNA
- RNase H domain whose role is to cleave RNA from DNA_RNA duplex.
- HBx Ag: The function of this protein is still unknown.
Genome:
- Genome is a circular ds DNA composed of 3200 nucleotide. One of the strand (+strand) is incomplete, hence the DNA appears partially ds and partially ss.
- DNA polymerase is associated with + strand which has both DNA dependent DNA polymerase and RNA dependent reverse transcriptase functions.
- Genome of Hepatitis B virus encodes four open reading frame (ORF).
- First ORF is Pre-S-S (pre-surface-surface):
- This ORF encodes three antigens obtained by differential initiation of translation at three different initiation codons.
- The three antigens are- HBs Ag, pre S2 (unknown function) and pre S1 (helps in virus attachment, assembly and release)
- Pre-core-core ORF (Pre-C-C):
- It codes for HBc Ag and HBe Ag. These are also overlapping and obtained by differential mutation of overlapping translation at two AUG codon
- When C-region is translated, core protein (HBc Ag) is formed and when translation begins from pre-C region to C-region, HBe Ag is formed.
- HBe Ag has no role in assembly
- Open reading frame P (ORF-P):
- It codes for viral DNA polymerase
- Open reading frame X (ORF-X):
- It codes for HBx Ag which acts as transcriptional trans-activator.
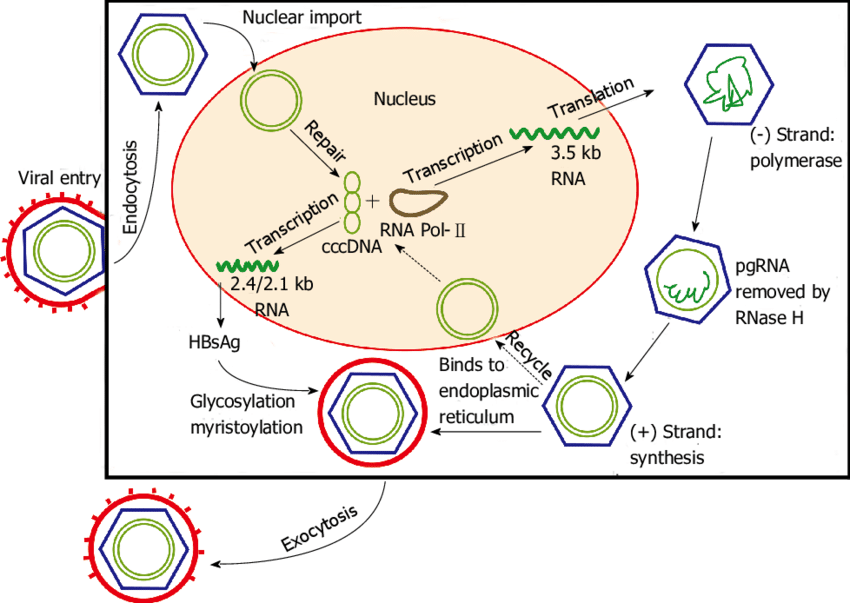
Replication of Hepatitis B virus:
- Hepatitis B virus is para-retro virus. The virus penetrates into host cell by binding to sodium taulocholate cotransprotein (NTTP) receptor.
- The virus penetrates the cell by endocytosis.
- The viral nucleic acid which is released by membrane fusion is then carried to the nucleus of host by chaperons.
- The partially ds DNA is then converted into covalently closed circular DNA (cc-DNA) which is a complete ds circular DNA.
- The viral DNA is then transcribed by RNA polymerase producing 4 mRNA (3.5kbp, 2.4kbp, 2.1kbp and 0.7kbp). One of which is intact and longer than virus DNA itself.
- The longest mRNA encodes for HBc Ag, HBeAg, and polymerase
- The other two mRNA encode for surface glycoproteins and the smallest mRNA (0.7kbp) encodes for X-protein (HBx) which is involved in virus replication and also helps in spread of virus.
- The mRNA are transported to the cytoplasm for translation and the proteins are produced.
- The surface proteins are localized in membrane Endoplasmic reticulum or golgi, from where virus eventually buds out after completion of replication
- The largest mRNA (3.5kbp) encapsidated along with viral polymerase with HBc Ag and HBeAg
- The polymerase synthesize single stranded DNA (-ve sense) from the RNA by its reverse transcriptase activity.
- The RNase H activity of the polymerase degrade RNA from RNA-DNA hybrid.
- The virus is then bud out form the ER and acquire the envelope containing the surface antigens.
- It is during this time or later +ve sense DNA is copied from the viral –ve sense DNA strand.
- This virion is then subjected to vesicular transport and is released by exocytosis from the membrane.
Mode of transmission of Hepatitis B:
- Hepatitis B is transmitted by the exchange of body fluids-blood, serum, semen, breast milk and in some circumstances saliva.
- Concentration of HBV in various body fluid:
- High: blood, serum, wound exudates
- Moderate: semen, vaginal fluids, saliva
- Low: urine, feces, sweat, tears, breast milk
- Transmission of HBV occurs by following routes:
- From infected mother to child
- Transfusion of HBV infected blood or blood products
- Sexual contact with infected person.
Pathogenesis of hepatitis B virus:
- Hepatitis B virus infection is an immune-pathological disease.
- HBV after entering the blood infects hepatocytes with the expression of viral antigen on the surface of infected cells. Copies of HBV genome integrate into hepatocyte chromosome and remain latent.
- Viral DNA and HBc Ag can be detected in nucleus while HBs Ag in cytoplasm and at hepatocyte membrane.
- The intracellular accumulation of filamentous form of HBs Ag produces the ground glass appearance of affected hepatocyte which is the characteristic feature of HBV infection.
- Adaptive immunity is more involved than the innate immunity in causing tissue destruction. Infact both tissue destruction and virus clearance from the host cell are attributed to cellular immunity (CMI)
- MHC I activated CD8 T-cell and MHC II activated CD4 T-cells are involved in pathology of disease. However most of the destruction is due to CD8 T cells.
- CD8 T cells also induce TNF-α and other cytokines including interferon-Ƴ which further compound the non-specific liver destruction.
Primary infection (acute infection):
- The incubation period of HBV is usually 4-10 weeks
- HBs Ag begins to appear in the serum during the incubation period and continues to increase. Its level can reach as high as 10,000 to 100,000 PEI (paul erlich institute). Its level begins to decline with the prodromal phase, disappear completely with appearance of symptoms and during recovery.
- Anti-HBc IgM antibody begins to rise with the onset of symptoms and this is the marker of acute infection.
- As HBs Ag become detectable, there is also marked increase in viral titer which can peak upto 109 to 1010 virions/ml.
- HBe Ag also become detectable. By this time 70-80% of liver cells are infected.
- Even if liver injury occurs, alanine aminotransferase level does not rise until and unless liver infection is well established. This reflects the amount of time required for T-cell response to initiate and attack the hepatocytes.
- Once the response begins, viral titers from liver and blood begin to decline.
- With clearance of virus, HBs Ag and HBe Ag level disappear. Subsequently level of anti-HBs Ag begins to rise.
- Even though HBs Ag and HBe Ag disappear with the appearance of anti- HBs Ag and anti-HBe Ag, it has been found HBV DNA persists. This HBV genome may not be enclosed within a virion or the genome is incomplete.
Chronic infection:
- A chronic carrier of HBV is an important event in the pathogenesis.
- Persistent infection of hepatocytes result in presence of HBV and HBs Ag in blood for at least 6 months. Whether an infected host cell will become a chronic carrier state or will be free of infection depends on the cytotoxic T-cell response.
Clinical manifestation:
- Clinical disease in susceptible host can be symptomatic or asymptomatic. Asymptomatic cases are more common in children.
- Infection in adults whether it is symptomatic or asymptomatic, is self-limited which may be due to virus clearance or immune response of individuals towards the virus.
Acute hepatitis B:
- It is characterized by gradual onset of anorexia, malaise and fatigue.
- During Acute (icteric) phase, the liver become tender with the development of jaundice, nausea, vomiting and passing of dark colored urine
Chronic hepatitis B:
- 5% of the adults may develop persistent infection.
- Persistent infection can also be symptomatic or asymptomatic.
- In people with sub-clinical persistent infection, normal level of serum amino-transferase and normal or nearly normal findings on liver biopsy indicates asymptomatic chronic persistent infection.
- However abnormal liver function test and histological findings on biopsies indicate symptomatic chronic persistent infection.
- Depending upon the extent of viremia and host response, chronic infection can lead to liver cirrhosis and hepato-cellular carcinoma (HCC).
- HCC usually occurs in association with cirrhosis. However in some case HCC has been found to occur independently.
- If the extent of virus infectivity is high chronic infection can also lead to glomerulonephritis and polyarthritis nodosa due to deposition of circulating immune complexes.
Lab diagnosis of HBV:
- The initial diagnosis of Hepatitis B is made on the basis of clinical features and laboratory findings on serum bilirubin and enzymes transaminase, ALT and AST
- Specimen: Blood, serum, body secretions
- Microscopy: Immunofluorescence staining:
- Immunofluorescence staining of infected hepatocytes show HBV core antigen in the nucleus and infectious Dane particle in cytoplasm.
- Molecular diagnosis:
- Detection of viral DNA by molecular methods such as insitu hybridization and PCR in tissue sample and serum reflects the degree of virus replication in liver.
- Serology:
- Appear Standard serological test of HBV is detection of HBs Ag.
- HBs Ag is the first marker to appear in blood after infection. It can be detected even before elevation of transaminase enzymes and onset of clinical symptoms.
- HBs Ag remains in blood circulation throughout the acute phase of disease.
- When HBs Ag is no longer detectable, its antibody (anti-HBs) appears and is detectable for longer period.
- Detection of IgM anti HBs indicates recent infection while detection of IgG anti-HBs indicates past infection.
- Presence of anti-HBs without other serological virus marker indicates immunity following vaccination.
- HBc Ag is not detectable in blood because it is enclosed within HBs Ag. But anti-HBc antibody appears in serum 1-2 weeks after appearance of HBs Ag.
- HBe Ag appears in blood concurrently with HBs Ag or soon afterwards. The disappearance of HBe Ag coincides with the fall of transaminase levels in blood which is followed by anti-HBe Antibody.
Treatment and Vaccines:
- Treatment of patients with hepatitis is supportive and directed at allowing hepatocellular damage to resolve and repair itself.
- Recombinant interferon-α and pegylated interferon-α are currently used in HBV treatment.
- Antiviral drugs: Nucleotide analogs (Lamivudine)
- Orthotopic liver transplant: It is the treatment for chronic hepatitis end stage liver damage
- Vaccine for HBV is available since 1982. Initially vaccine was prepared by purifying HBs Ag associated with 22 nm particle and inactivating through formalin treatment.
- Recombinant HBs Ag produced by recombinant DNA technology using yeast cell or mammalian cell line culture is used as first recombinant vaccine.
- Passive immunization using specific hepatitis B immune globulin (HBIG) have shown effective protection. However it is not recommended for pre-exposure prophylaxis.
