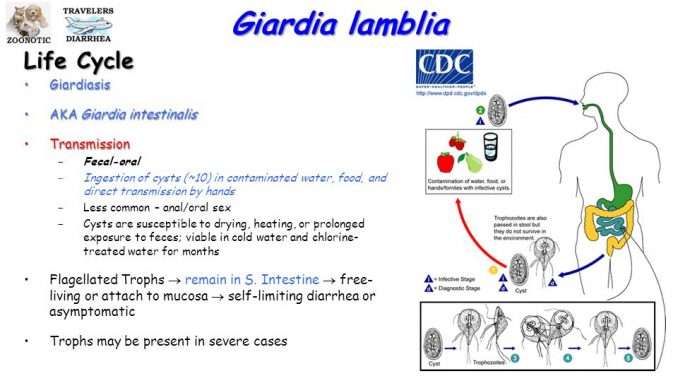
Giardia lamblia: Morphology, life cycle, pathogenesis, clinical manifestation, lab diagnosis and treatment
- Giardia lamblia is also known as intestinilis or G.duodenalis.
- It was first observed by Antony von Leewenhoek (1681) while examining his own stool and Lambi (1859) describe the parasite and named it as Giardia labmlia
- Giardia is the only intestinal flagellate known to cause endemic and epidemic diarrhea in human.
Habitat:
- Inhabits the small intestine of human
Morphology:
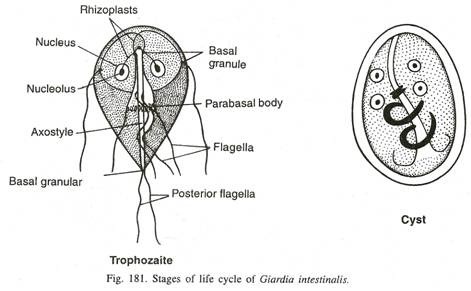
G. lamblia exists in two morphological form- trophozoite and cyst
-
Trophozoite:
- It is the active feeding stage of parasite which is responsible for colonization in intestine.
- The shape of trophozoite is pear shape or tennis racket shape with broad round anterior end and a tapering posterior end.
- It measures 9-21 µm in length and 5-5µm in breadth.
- The dorsal surface is convex while ventral surface is concave with a sucking disc (adhesive disc) which acts as an organ for attachment.
- Behind the adhesive disc lies a pair of large curved and transverse median bodies, unique to
- It is bilaterally symmetrical and all organs of body are paired. They have two median bodies, two axostyle, two nuclei and four pairs of flagella.
- Each nucleus consists of large central karyosome giving a characteristic face like appearance to the parasite in stained preparation.
- Cytoplasm is uniform and finely granulated.
- Motility shown typical ‘fallling leaf type’ motility.
-
Cyst:
- It is an infective stage of parasite.
- A fully mature cyst is oval or ellipsoidal in shape and measures 8-12µm in length and 7-10µm in breadth.
- Cyst is surrounded by a thick cyst wall. Cytoplasm is granulated and is separated from the cyst wall by clear space.
- The axostyle lies more or less diagonally.
- A cyst contains 4 nuclei.
- The remaining of flagella and the margins of sucking disc may be seen inside the cytoplasm.
Life cycle of Giardia lamblia:
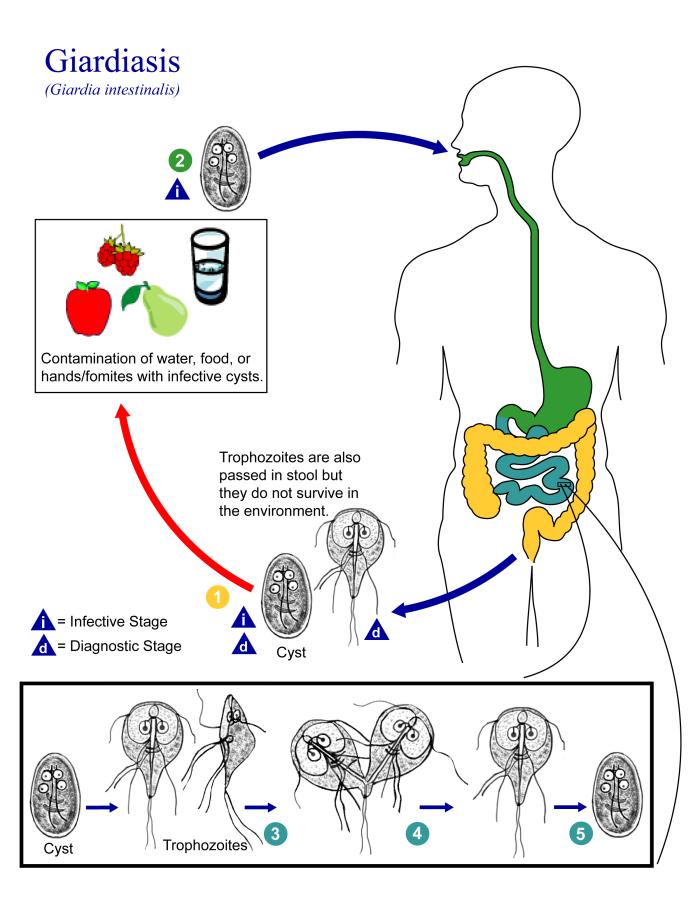
- Life cycle of G. lamblia is simple and completes in a single host, man. No intermediate host is required.
- Infection is acquired orally by ingestion of cyst from contaminated hand or water or food.
- Excystation occurs in th stomach and in the duodenum in the presence of gastric acid, pancreatic enzymes (chymotrypsin and trypsin). An acidic environment with a pH 1.3-2.7 is required for excystation.
- Each cyst excysts to produce two trophozoites in the duodenum within 30 minutes of ingestion.
- These trophozoites multiplies in the intestine by bunary fission. Then they adhere to enterocytes through their ventral sucker mediated possibly through surface mannose-binding lectin present on the surface of trophozoites.
- Some of the trophozoites then pass down on the large intestine where they again encyst in the presence of neutral pH and bile salts.
- The process of encystation begins with the appearance of encystation specific secretory vesicles (ESVs) in the cytoplasm of trophozoites, followed by production of cyst wall within 15 hours.
- Within 24 hours after appearance of ESVs, the trophozoite is covered with these cyst wall proteins, resulting in formation of cyst.
- Formation of cyst begins by shortening of flagella followed by condensation of cytoplasm and finally secretion of thick hyline cyst wall.
- These encysted trophozoites then undergo another phase of nuclear division and produces quadrinucleated mature cyst.
- The cysts which are the infective form of parasite are excreted in faeces and life cycle is repeated.
Pathogenesis and pathology:
Mode of transmission:
- Man is the main reservoir of Giardia.
- Infection is acquired due to-
- Ingestion of contaminated food and water
- Person to person transmission due to poor hygiene in day care centers, nursing homes, mental asylums
- Sexual transmission-oral-anal and oral-genital sex
- Immunocompromised individuals such as AIDS patients, X-linked gammaglobulinaemia, patients with protein energy malnutrition are more susceptible for giardiasis
Virulence factors:
- Cytoskeleton:
- Giardia contains microtubules (MT) cytoskeletion which is essential for motility, attachment, intracellular transport, cell division and encystation/excystation.
- Cysts:
- Cysts are resistant and responsible for transmission of parasite
Pathogenesis of Giardia lamblia:
- Giardia is intestinal parasite and it is non-invasive.
- Once excystation occurs, trophozoites are releases and they uses their flagella to ‘swim’ to the microvilli covered surface of duodenum and jejunum where they attach to the enterocytes using their adhesive disc.
- Lectins present on the surface of Giardia binds to receptor present on surface of enterocytes. This attachment process damage microvilli, which interfere with nutrition absorption by villi.
- Rapid multiplication of trophozoites eventually creates a physical barriers between the enterocytes and intestinal lumen, further interfering with nutrition absorption. This process leads to enterocytes damage, villi atropy, crypt hyperplasia, intestinal hyperpermeability and brush boarder damage that causes a reduction in disaccharide enzyme secretion.
- Lectins and othere cytopathic substance secreted by parasite also causes indirect damage to intestinal epithelium.
- Trophozoites do not invade or penetrate surrounding tissue or enter blood stream. So, infection is generally restricted to intestinal lumen.
- Giardiasis results in decreased jejunal electrolyte water and glucose absorptiom, and damages to intestinal epithelium leads to malabsorption of electrolyte and fluids, resulting in osmotic diarrhea known as giardiasis.
Clinical manifestation of Giardia lamblia:
- Incubation varies from 1-3 weeks
- In majority of cases infection remains asymptomatic.
- Symptomatic infection is more common in children than adults because of their lower immunity.
-
Acute giardiasis:
- It is characterized by acute watery diarrhea, abdominal cramp, bloating and flatulence. Occasionally nausea, vomiting, fever, rashes or constipation in some.
- Pus, blood and mucus are not seen in stool.
- The condition lasts for 5-7 days.
-
Chronic giardiasis:
- Symptoms includes chronic diarrhea with malabsorption of fat (steatorrhoea) and malabsorption of vitamin A, protein and D-xylose, weight loss, malaise, nausea, anorexia
- Protuberance of abdomen, spindly extremities and stunted growth are most common sign in children.
- It lasts for several weeks
- Extra-intestinal are rare and sometimes urticarial and reactive arthritis are seen in rare case
-
Complication:
- In adults, malabsorption syndrome and weight loss
- In children, growth retardation, delayed milestones achievements
- Giardiasis is self-limited disease and progression to chronic state is only 5% of infected people and death is rare.
Laboratory diagnosis of Giardia lamblia:
-
Specimen:
- Stool, duodenal contents, bile stained mucus, duodenal/jejunal biopsy
-
Stool examination:
- Microscopy:
- Direct wet mount preparation: trophozoites are identified by their characteristic falling leaf motility
- Iodine wet mount preparation: cyst can be observed
- Examination of stained stool smear for demonstration of trophozoitse
- Concentration method: formalin-ethyl acetate and zinc sulfate concentration method is used to concentrate stool and increase parasite yield for microscopy
- Stool antigen detection: ELISA, IFA
- Microscopy:
-
Stool culture
-
Entero-test:
- In entero-test, a gelatin capsule containing a nylon string with a weight attached to it is swallowed by patients.
- When it reaches to stomach, the gelatin capsule is diddolved and nylon string moves down to duodenum and jejunum due to its attached weight.
- The string is allowed to remain there for 4-6 hours or overneight.
- After removal of string, bile stained mucus is collected on glass slide and examined for living trophozoites.
-
Serology
-
Molecular methods
Treatment for giardiasis:
- Metronidazole, trinidazole, nitroimidazole derivatives
- Nitrofurans- furazolidine
- * metronidazole is drug of choice. Dose- orally 250mg, 3 times daily for adults, 15mg/kg /day in three divided dose for children for 7 days
Prevention of giardiasis:
- Improve water supply
- Proper disposal of human faeces
- Maintenance of good and proper personal hygiene
- Health education at individual as well as community levels
- Identifying the source of infection, particularly in outbreak situation
Giardia lamblia: Morphology, life cycle, pathogenesis, clinical manifestation, lab diagnosis and treatment
