Dengue pathogenesis, clinical manifestation, lab diagnosis and treatment
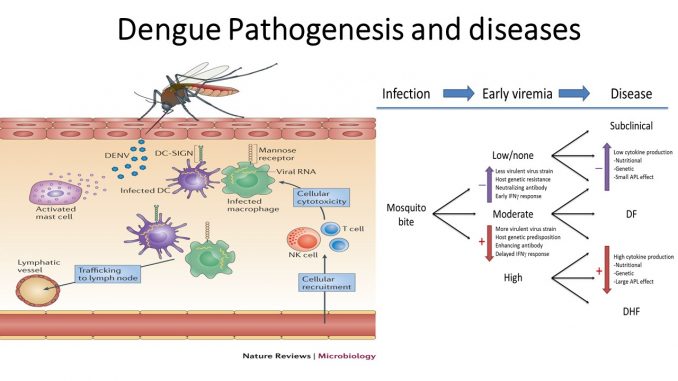
Pathogenesis of Dengue:
- Dengue virus after entering in the body invades the local macrophages and multiply there.
- Infected local cells then migrate from site of infection to lymph nodes, where monocytes and macrophages are recruited, which become targets of infection.
- Consequently, infection is amplified and virus is disseminated through the lymphatic system. As a result of this primary viremia, several cells of the mononuclear lineage, including blood-derived monocytes
- Viremia develops within 24 hours. During this period, virus travels throughout the body.
- Bone marrow cells have also been shown to be susceptible to infection with DENV
- In severe case, viral load is very high and many vital organs are affected.
- Virus infected macrophages produces a number of signaling proteins such as interferons, cytokines, chemokines, TNF, other mediators which are responsible for many symptoms such as flue like syndrome and pain.
- These mediators affects hemostatic system of body.
- Fluid from blood vessels starts to leak out so that the blood volume decreases resulting in low blood pressure.
- Decrease in blood pressure causes insufficient supply of blood and Oxygen to vital organs such as brains.
- Dengue also infects bone marrow, so that bone marrow cannot produces sufficient platelets.
- Since platelets are needed for blood clotting, dengue infection causes blood clotting defect and increase the risk of bleeding.
Primary infection:
- Primary infection is characterized by fever, break bone fever, retro-orbital pain and flue like syndrome.
- The person who is not previously infected with any Flavivirus is termed as primary infection.
- In primary infection ratio of Dengue specific IgM to IgG is high.
Secondary infection:
- Dengue infection in host who is immunologically sensitized to dengue or other flavivirus is termed as secondary infection.
- Secondary infection is characterized by rise in antibody titer. The ratio of IgM to IgG is low.
Clinical manifestation:
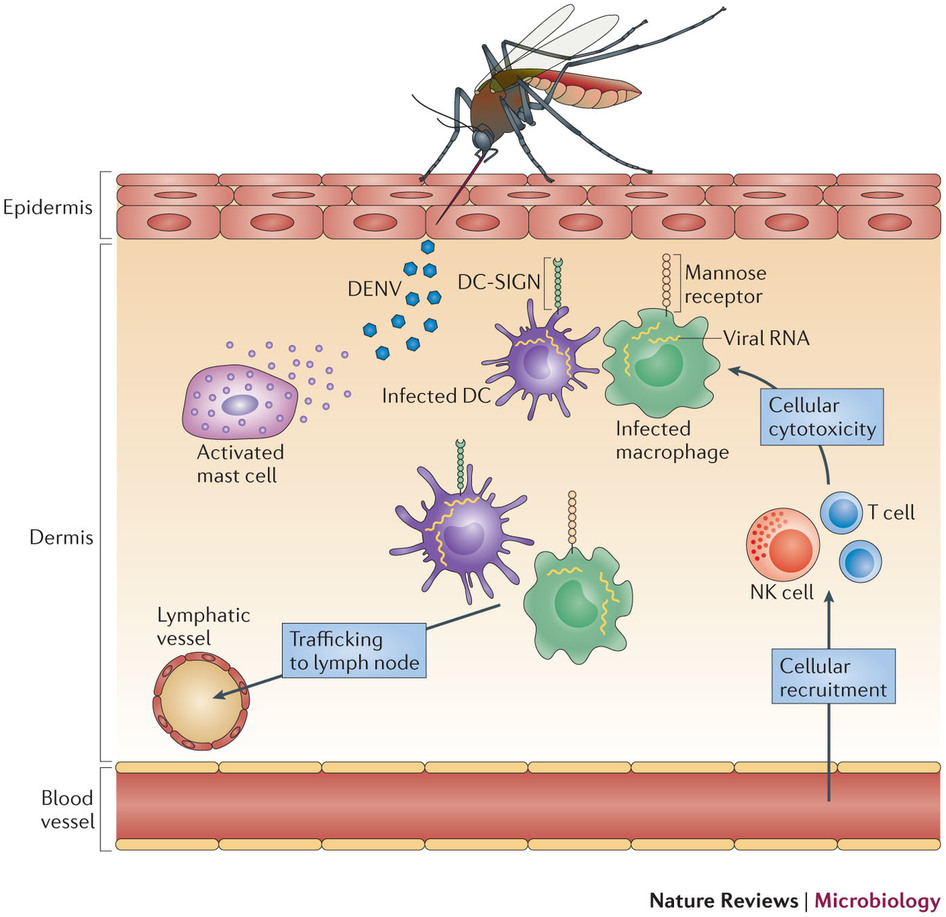
- Dengue fever is symptomatic or asymptomatic.
- Clinical disease onsets 4-6 days after infective mosquito bite.
Symptomatic dengue includes, classical dengue fever, Dengue haemorrhagic fever (DHF) and Dengue shock syndrome (DSS).
I. Classical dengue fever:
- It is characterized by fever, rashes, severe headache, pain behind eyes, pain in muscle and joints, enlarged lymph nodes,
- Fever lasts for 2-7 days
- Myalgia and break bone fever ( deep bone pain) is the characteristic of Dengue fever
- Classical dengue fever is self-limited.
- Mostly adults and older children are affected,
II. Dengue hemorrhagic fever (DHF):
- DHF is marked by bleeding from skin and mucus membrane.
- DHF has four major clinical manifestation- High fever, hemorrhagic phenomenon, hepatomegaly and circulatory failure.
- In early stage of infection DHF resembles classical dengue fever.
- Usually occurs in children
- About 23% of children with DHF develops circulatory failure with haemo-concentration and a marked decrease in platelets counts leading to severe hemorrhage.
III. Dengue shock syndrome (DSS):
- DSS is serious form of DHF.
- All serotypes of Dengue are associated with DHF and DSS.
- The cause of DSS is not clearly understood. But it is assumed due to antibody dependent enhancement (ADE).
- Pre-existing heterologous antibody against particular dengue serotype binds with the new infected virus serotype by its Fab region and Fc region of antibody binds to receptor on macrophage. So this pre-existing antibody increases virus infection to healthy macrophages.
- From recent outbreak information of DHF, patients infected with DEN-2 after primarily infected with other serotypes can leads to DSS.
- DSS is characterized by circulatory failure, rapid pulse, abnormal pain, severe bleeding from GI tract and other organs.
- Usually occurs in children
Lab diagnosis:
Sample: blood, serum
-
HIA (Hemagglutinin Inhibition assay): test antibody against hemagglutinin spike of virus.
-
FAT (Fluorescence antibody test): detects virus antigen using virus specific antibody
-
MAC-ELISA (IgM capture ELISA): detects Dengue specific IgM antibody.it can distinguish primary infection from secondary infection. In primary infection ration of IgM to IgG is greater than 1.5
-
Neutralization test: detect antibody against dengue
-
Virus isolation: mosquito cell line culture with patient serum.
-
Nucleic acid detection: RT-PCR is used to detect virus genome.
Treatment:
- No specific treatment for dengue.
- Early and proper diagnosis can reduce symptoms and prevents complication and death
- Vaccine:
- Dengvaxia vaccine is licensed and available in some countries for people ages 9-45 years old. The World Health Organization recommends that the vaccine only be given to persons with confirmed prior dengue virus infection.
- The vaccine manufacturer, Sanofi Pasteur, announced in 2017 that people who receive the vaccine and have not been previously infected with a dengue virus may be at risk of developing severe dengue if they get dengue after being vaccinated.
