Chronic obstructive pulmonary disease (COPD)
What is COPD?
- Chronic obstructive pulmonary disease COPD are commonly used clinical terms for a group of pathological condition in which there is chronic, partial or complete obstruction, to the airflow at any level from trachea to the smallest airway resulting in functional disability of the lungs.
- The following 4 disease condition are included in COPD
- Chronic bronchitis
- Emphysema
- Bronchial asthma
- bronchiectasis
- In COPD, less airflow in and out of the airways because of one or more of the following
• the airway and the air sacs lose their elastic quality
• the walls between many of the air sacs are destroyed.
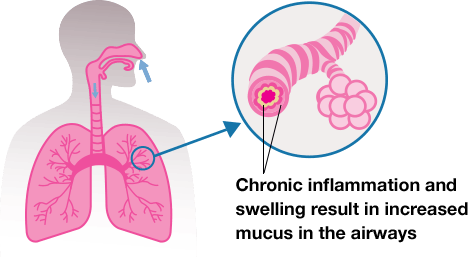
• The wall of the airways become thick and inflamed.
• The airways makes more mucus than, usual which tend to clog them.
What are the causes of COPD?
Causes of COPD
- Long term exposure to lung irritant that damage the lungs and the airway
- Most common irritant that cause COPD is cigarette smoke
- Exposure to fumes from burning fuel
- People with asthma
- In rare case, a genetic condition called alpha-1antitrypsin deficiency may cause
What are the risk factors of COPD?
Risk factor of COPD
- People who smoke or are exposed to smoke.
- Family history of COPD are more likely to develop the disease if they smoke.
- Long-term exposure to other lung irritant also is a risk factor.
- Almost 90% of COPD death occur in low and middle income countries, where effective strategies for prevention and control are not always implemented or accessible.
Sign and symptoms of COPD
- Feeling of oxygen deprive
- Breathlessness
- Sputum mix with saliva and mucus and may be clear, white, yellow, or greenish
- Chest tightness
- Trouble taking a deep breath
- Unintended weight loss in later stage
- Frequent chest infection
- Wheezing
Diagnosis of COPD
- History taking
- Physical examination
- Spirometry to measure how much air a person can exhale and inhale and how fast air can move into.
- Chest x-ray
- CT scan of chest
How can you manage COPD in hospital?
There are 3 ways to manage COPD
1. Medical management
2. Surgical management
3. Nursing management
MEDICAL MANAGEMENT
• Inhaled bronchodilator
• Β-agonists ( relax bronchial smooth muscles and increase mucociliary clearance)
• Anticholinergic that relax bronchial smooth muscle through competitive inhibition of muscarinic receptor ( M1, M2, M3)
• Oxygen therapy
• Corticosteroid and Nonsteroidal anti-inflammatory drug (NSAID)
• Palliative measure such as regular exercise, good nutrition, flu and pneumonia vaccines
SURGICAL MANAGEMENT
• Lung volume reduction surgery: to remove damage lung tissue
• Bullectomy: removal of large bullae that does not contribute to gas exchange or responsible for complications
• Lungs transplant: to improve health status, functional capacity but does not prolong survival in selected patient with very severe COPD
NURSING MANAGEMENT
Assessment
- History of smoking, family history, occupational history
- Arterial Blood gas (ABG) analysis
- Respiratory rate, depth and characteristics
- Sputum amount and type
- Anxiety level of the patient
- Inspect the use of accessory muscle during respiration and use of abdominal muscle during expiration
Nursing Diagnosis
- Ineffective breathing pattern related to chronic airflow limitation
- Ineffective airway clearance related to bronchoconstriction, increased mucus production, ineffective cough, possible bronchopulmonary infection
- Risk of infection related to compromised pulmonary function, retained secretions and compromised defense mechanisms
- Imbalanced nutrition less then body requirement related to increased work of breasting, presenting dyspnea and drug effect
- Deficient knowledge of self-care strategies to be performed at home
Intervention
- Monitor vitals and general condition of the patient
- Give medication as per cardex
- Monitor pulse oxymetry
- Monitor lung sound every 4 to 8 hours
- Perform chest physiotherapy
- During acute episodes, open door and curtains and limit the numbers of people in the room
- Encourage the use of breathing retraining and relaxation technique
- Give sedative and tranquilizer with extreme caution
- Assess skin color and temperature
- Keep the patient in flowers position
- Advice the patient to drink at least 8 to 10 glasses of fluid per day unless contraindicated
- Asses the condition of oral mucus membrane and provide oral care
- Provide knowledge about disease condition and progress
- Provide proper nutrition aids in the prevention of secondary respiratory infection
- Encourage smoking cessation if applicable
