Herpes simplex virus(HSV): structure and genome, mode of transmission, pathogenesis, infection, laboratory diagnosis and treatment
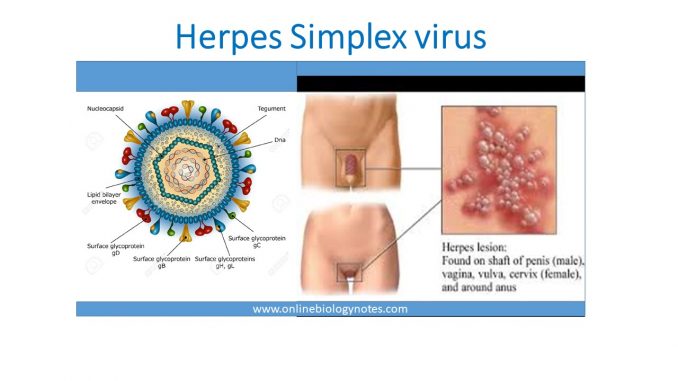
Structure and genome
- HSV is large enveloped icosahedral virus
- Human is only natural host for HSV. It is also known as Human Herpesvirus.
- HSV are of two types: HSV1 and HSV2. Two viruses are structurally and morphologically similar. However they are distinguished antigenically by using type specific monoclonal Ab, restriction endonuclease pattern of their genome, and site of lesions
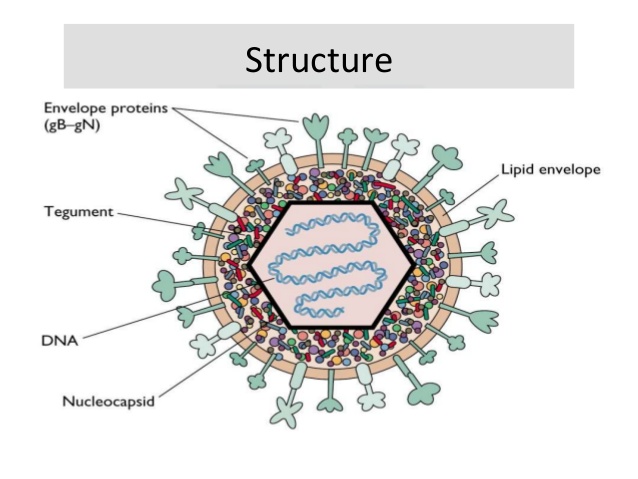
- Size: 120-200nm in diameter
- Genome: linear ds DNA
- Enveloped
- Replication and assembly occur in nucleus of infected cell
Mode of transmission:
- Direct contact with lesion fluid or saliva
- Sexual transmission; genital herpes
- Perinatal route; child gets Herpes during birth from infected mother
- Congenital transmission; it is rare
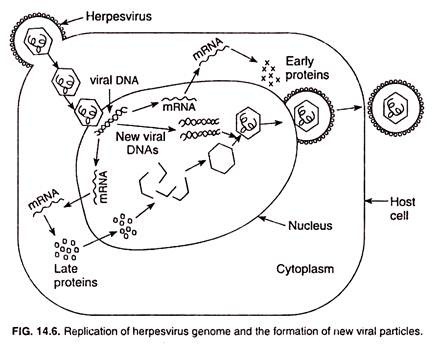
Replication cycle:
Pathogenesis:
- Virus enter through skin and mucus membrane and multiply locally
- Virion interacts with specific cell surface receptor through its glycoprotein spike
- HSV1 and HSV2 have several cell surface receptor, they uses one of them for entry in host cell
- Binding of glycoprotein trigger fusion of viral envelope with host cell membrane and this fusion causes the release of nucleo-capsid into cytoplasm and is transported to nucleus.
- In the nucleus of host cell, virus replication occur immediately. At first Viral gene will be transcribed leading to synthesis of virus protein, replication of virus genome and assembly of progeny viruses.
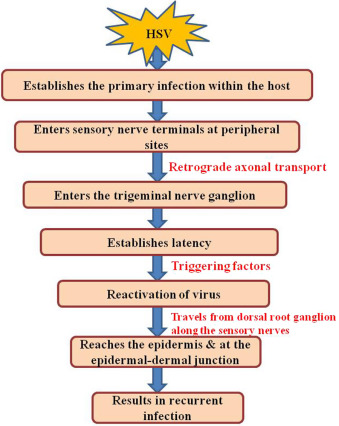
1. Primary infection:
- HSV1 infection are usually limited to oropharynx and transmitted by respiratory droplet or saliva whereas HSV2 infection usually transmits by genital route.
- Primary infection of Herpes results in vesicle formation under the layer of keratinized squamous epithelium cell. The vesicle is filled with fluid which contains multinucleated giant cells and eosinophilic intranuclear inclusions bodies along with inflammatory cell and cellular debris
- After primary infection, the virus invades local nerve ending and travel from retrograde intra axonal flow to sensory root ganglia where they further multiply.
- The virus settle within neuron in sensory ganglia (trigeminal ganglia in case of HSV1 and sacral ganglia in case of HSV2) and remain latent.
2. Latent infection:
- During latency no viral particles are produced. Also the latent infection does not causes any demonstrable damage in neuron.
- This latency phase may be reactivated periodically in some individuals causing recurrent oral and genial lesion.
3. Recurrence herpes:
- Various stimulus such as physical or emotional stress, trauma, fever, sunlight, certain food, menstrual cycle in female etc can induce recurrence of latent infection.
- In recurrence the virus travels back from neuron and multiply in mucosal epithelial cell producing lesion at the same spot each time.
- The recurrent infection can also occurs in presence of specific antibodies. However recurrent infection are less severe, more localized and of shorter duration than that of primary infection due to presence of past immune response.
- As a general rule HSV-1 produce lesion above waist and HSV-2 below waist. But the rule is not absolute.
- The lesion of HSV are thin walled, umbilicated which break causing superficial ulcer and heal without scaring.
Clinical manifestation:
- Clinical manifestation and course of disease depends upon site of infection, age and immune status of host as well as antigenic type of Herpes virus.
1. Cutaneous or skin infection:
- It is characterized by fever blister or herpes febrilis on face, cheeks, chin, around mouth and forehead.
- It occurs by reactivation in febrile patients by certain stimulus such as stress, common cold, exposure to sun etc.
- Generalized eruption of lesion over body may occurs in children suffering from eczema.
- Herpetic whitlow is an occupational cutaneous herpes seen in doctors, dentists and nurses.
2. Mucosal or Oropharyngeal infection:
- Gingivostomatitis and pharyngitis are frequent.
- Acute Gingvostomatitis is the primary HSV-1 infection occurring in children between 6 month to 5 years old.
- It is characterized by vesicular lesion on oral mucosa, tongue and lips. The lesions subsequently rupture and coalesce together leaving behind ulcerated plaques.
- Pharyngitis and tonsillitis manifests with fever, malaise, headache and sore throat.
3. Ophthalmic or eye infection:
- Keratoconjunctivitis
- Follicular conjunctivitis
- Corneal blindness
- Chorioretinitis and acute necrotizing retinitis
4. Nervous system infection:
- Herpes encephalitis; caused by HSV-1
- Herpes meningitis; caused by HSV-2
- Autonomic dysfunction of nervous system
- Guillain-barre syndrome
- Bell’s palsy
5. Visceral herpes:
- Herpes esophagitis
- Tracheobronchitis
- Pneumonitis
- Hepatitis
6. Genital herpes:
- It is mostly caused by HSV-2
- Primary genital herpes is asymptomatic caused by both HSV-1 and HSV-2. Recurrent is more frequent in HSV-2
- In male lesions appears in glans or shaft and occasionally on urethra.
- In female lesions appears on valve, vagina, cervix, perianal area
- In both sexes, genital herpes is characterized by fever, pain, dysuria, mucoid urethral discharge with enlarged inguinal lymph node,
7. Congenital herpes:
- Transplacental transmission leads to congenital infection but it is rare.
- Neonatal herpes is caused by HSV-2, and it is manifested as infection of eye, mouth, skin and more commonly a disseminated infection with multiple organ involvement.
- Mortality rate is high and survivors may have neurological disabilities.
Laboratory diagnosis:
1. Specimens:
- Saliva, vesicle fluids, conjunctival fluids, corneal scrapping, skin swab and CSF.
- Depends upon site of infection
2. Microscopy:
- Tzanck smear preparation: Smear is prepared from lesion and stained with 1% aqueous solution of toluidine blue for 15 seconds. Multinucleated giant cells are visualized in positive smear.
- Giemsa stain can also be used to see inclusion bodies.
3. Electron microscope
4. Virus Culture:
- Primary human embryonic kidney cell line culture, Hela cell, Human amnion, Hep2
- Cytopathic effect should be visualized within 1-3 days
5. Serology:
- ELISA, neutralization test, Complement fixation test (CFT), Immunofluorescent test
7. Molecular diagnosis:
- PCR, DNA probe
Treatment:
- Acyclovir; orally or parenterally
- Ganciclovir, Viderabine, Famiciclovir; orally
- Idoxuvidine; topically in eye and skin infection
Herpes simplex virus(HSV): structure and genome, mode of transmission, pathogenesis, infection, laboratory diagnosis and treatment
