HIV/AIDS: Replication, pathogenesis, clinical manifestation and lab diagnosis
HIV Replication
-
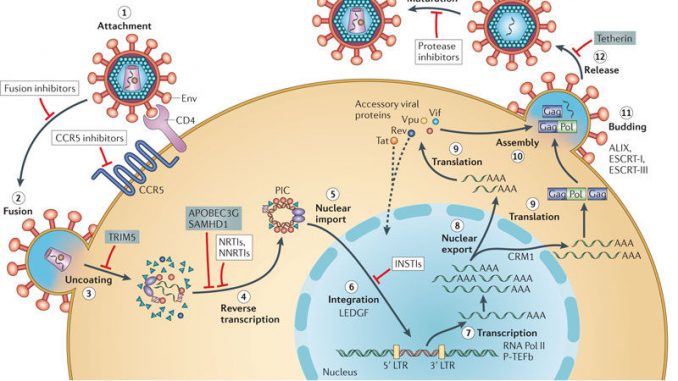
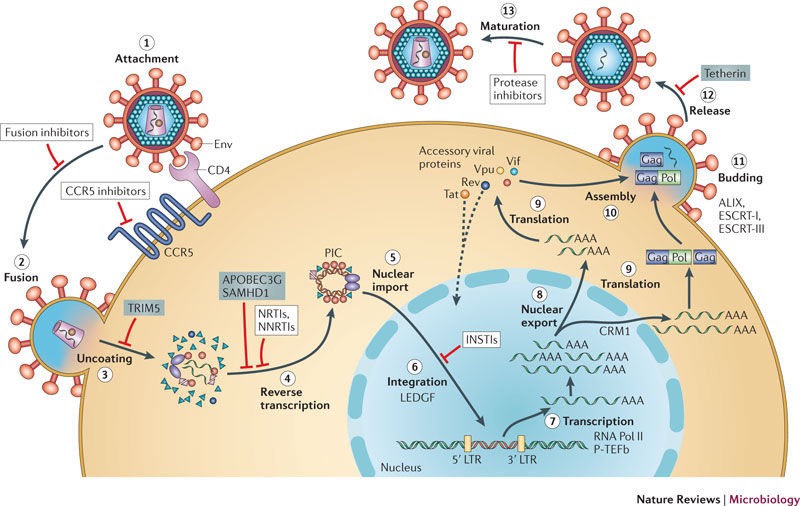
HIV uses CD4 molecule as a receptor which is present in CD4+ cells such as T-lymphocytes, macrophages, monocytes, dendritic cells other and Antigen presenting cells.
-
A second co-receptor in addition to CD4 molecule is required for HIV to gain entry into host cell. CCR5 for macrophage tropic HIV and CXCR4 for T-lymphocyte tropic HIV.
-
HIV first binds to CD4 molecule mediated by surface glycoprotein gp120 and then to the corresponding co-receptors CCR5 or CXCR4. This binding brings conformational change in viral envelope inducing the binding of gp41 of virus into host cell membrane and triggering the entry of virus into host cell.
-
Once the fusion of virus takes place with the host cell, viral RNA is released into the cytoplasm.
-
Viral RNA is then used to synthesize ds DNA by the enzyme reverse transcriptase (RNA dependent DNA polymerase). The ds DNA is then circularized and enter into host cell nucleus.
-
This circular ds DNA get integrated with host genome and the process is catalyzed by the enzyme integrase. This type of integrated viral DNA into host DNA is known as Pro-virus.
-
Once the viral DNA is integrated, infection of HIV is permanent.
-
The HIV virus may then enter into latency or enter into productive cycle.
-
In productive cycle, the pro-virus DNA is then transcribed into mRNA by host RNA polymerase and finally translated to viral proteins. These viral proteins are processed to form virion components which are then assembled.
-
The progeny virus now mature and release by budding.
-
During budding, it acquire envelope.
-
The released progeny virus infects suitable host cell and continues the productive cycle.
Pathogenesis of HIV/AIDS
Pathogenesis of HIV can be described under following headings.
1. Mode of transmission:
HIV infection is acquired through one of the following routes.
- Sexual contact; infected partner
- Parental route; infected needles or syringes
- Congenital route; infected mother giving birth
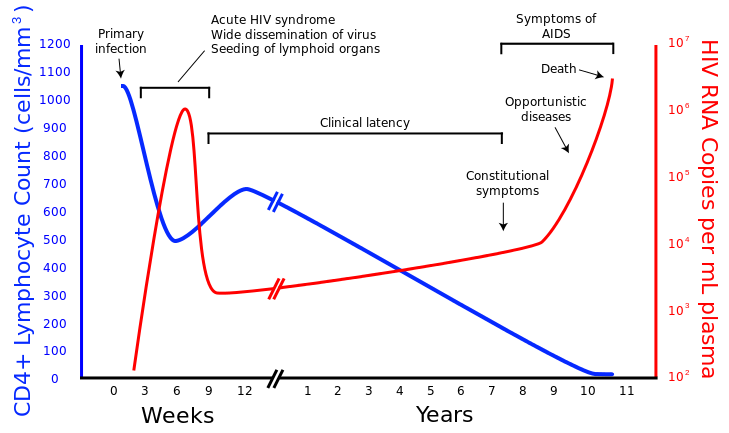
2. Primary infection: (acute infection):
- Once HIV enters the body through any of those routes they bind to CD4+ cells with their glycoprotein spikes and infect the cell. Thus the infection is established.
- HIV multiply in mucosa and there is 4-11 days between mucosal infection and initial viremia. Viremia is detectable for about 8-12 weeks.
3. Dissemination of virion to lymphoid organs:
- Virus from blood is then disseminated throughout the body and seeded in lymphoid organs.
- In this stage, it leads to acute mononucleosis like syndrome
- The CD4 T- cells count drop significantly during this time.
4. Clinical latency:
- An immune response to HIV develops 1 week to 3 months after infection, which leads to significant drop in viral load and rebounce of CD4 T-cells.
- The immune response however is unable to clear the HIV completely.
- The HIV infected cells persists in lymph nodes leading to clinical latency.
5. Elevated HIV level:
- The period of clinical latency lasts as long as for 10 years.
- During latency virus replication continues. Consequently patients develop constitutional symptoms and clinical diseases such as opportunistic infections, neurological disorder and neoplasm.
6. Clinical disease and death:
- The duration between primary infection and progression to clinical disease is 10-12 years while death occurs usually within 2 years after unset of clinical disease ie. AIDS in untreated cases.
Clinical manifestation of HIV/AIDS
1. Acute retroviral syndrome (ARS):
- It can occurs few days to few weeks after primary infection.
- It is found in 50-70% of infected patients.
- It is characterized by clinical signs of immune activation and multi system dysfunction
Symptoms includes;
- acute mononucleosis like syndrome
- fever
- generalized lymphadenopathy
- sore throat
- fatigue
- weight loss
- rashes,
- nausea
- night sweat
- occasionally diarrhea
- pancreatitis
- bacterial sepsis
- epiglottitis
- self limiting neurological disorder,
- meningitis,
- encephalitis.
All these symptoms resolves within 5-30 days.
2. Clinical latency and incubation to AIDS
- ARS is followed by long period of clinical latency which is free of any clinical symptoms
- Clinical latency is maintained because of host immune response against HIV
- The median time to develop AIDS in untreated cases is 10-12 years.
- 5-10% of patients are rapid progressors and they develops AIDS within 2-3 years
- Similarly, 5-10 % other patients are non-progressors and they become free of symptoms after 7-8 years.
- In congenital infection clinical symptoms usually appears by 2 years of age and death occurs in next 2 years.
3. AIDS:
- Significant drops in CD4 T-cells count (below 200 cells/µl) leads to AIDS.
- AIDS results in loss of ability to respond to infections.
- Loss of immune response immune response develops opportunistic infection and tumors
- Other clinical symptoms are; Tuberculosis, Parasitic infection, Hepatitis, oral hairy leukoplankia, Kaposi sarcoma, Dementia complex and other neurological symptoms.
Lab diagnosis:
-
Serology: detection of anti-viral antibody using ELISA. This test detects serum antibody against gp120, gp41, P24 etc. The first positive result must be confirmed by at least 2 other different assays with different viral antigen.
-
Western blotting: It is a confirmatory test.
-
RT-PCR: detection of RNA and DNA sequence of HIV
-
Virus isolation: culturing on CD4 + T-lymphocyte cell line